Published: October 26, 2022
Center for Field Epidemic Intelligence, Research and Professional Development,
National Institute of Infectious Diseases
Center for Surveillance, Immunization, and Epidemiologic Research,
National Institute of Infectious Diseases
We would like to express our deepest condolences to the bereaved families of all those who have passed away after SARS-CoV-2 infection.
Background and objectives
The Ministry of Health, Labour, and Welfare (MHLW) requested local public health authorities to conduct genome analysis of severe and fatal cases of SARS-CoV-2 infection to accumulate and monitor knowledge on the severity of SARS-CoV-2 infection on the basis of “the enhanced field epidemiological investigation requested for conducting genome analysis and variant screening by real-time polymerase chain reaction (PCR) tests for SARS-CoV-2 (Administrative notice #0205-4 from the Director of Tuberculosis and Infectious Disease Control Division, Health Serviced Bureau of MHLW on February 5, 2021; partially revised on February 10, 2022)” and “Regarding the handling of hospital admissions and discharges, close contacts, and disclosure of patients with confirmed infection by the B.1.1.529 lineage (Omicron variant) (Administrative notice from MHLW on February 2, 2021)” promulgated by Article 15, the Act on the Prevention of Infectious Diseases and Medical Care for Patients with Infectious Diseases (Act No. 114 of October 2, 1998).
Recently, the MHLW and the National Institute of Infectious Diseases (NIID) have been concerned about the severe or fatal pediatric cases of SARS-CoV-2 infection as the number of pediatric cases increased 1), so we conducted an epidemiological investigation of fatal cases of SARS-CoV-2 infection in patients under 20 years old (fatal pediatric cases). Fatal pediatric cases included those caused both directly and indirectly by SARS-CoV-2 infection. We collaborated with three academic societies: the Japan Pediatric Society, the Japanese Society of Intensive Care Medicine, and the Japanese Association for Acute Medicine.
This record is an interim analysis of the fatal pediatric cases reported from January 1 to August 31, 2022.
Methods
Subjects who satisfied either of the following two conditions were included in the investigation. Research staff or fellows of the Field Epidemiology Training Program for NIID collected epidemiological data of local health authorities and visited medical institutions to collect data on medical records if possible and interview physicians (hereafter, field investigation).
Subjects investigated
1)Patients under 20 years old whose date of onset (or admission date) was on January 1, 2022, or later, and who died during the acute phase of infection with SARS-CoV-2.
2)Patients under 20 years old whose date of onset (or admission date) was on January 1, 2022, or later, and who died after the acute phase of infection with SARS-CoV-2 (including cases with other causes of death).
Items investigated
Age, sex, underlying disease, vaccine history of SARS-CoV-2 immunization, date of onset, date of death, symptoms/findings, disease suspected of causing death, and others.
Results (Interim)
A summary of the cases and results of the field investigation as of August 31, 2022, follows below. In collecting the information on the cases, it was difficult to classify the subjects into those exactly meeting criterion 1) or 2). Moreover, we have taken care to ensure that individuals are not identifiable.
〇 Summary of the cases
The total number of cases was 41 (age: <1 year old, n=8 [20%]; 1–4 years old, n=10 [24%]; 5–10 years old, n=17 [41%]; 12–19 years old, n=5 [12%]; and unknown, n=1 [2%]; sex: males, 23 cases [56%] and females, 18 cases [44%]). The figure shows the distribution of cases based on the date of onset after January 1, 2022 (epidemiological week 52, 2021). Cases have been continuously reported since January 2022 and started to increase from epidemiological week 28 (July 11–July 17).
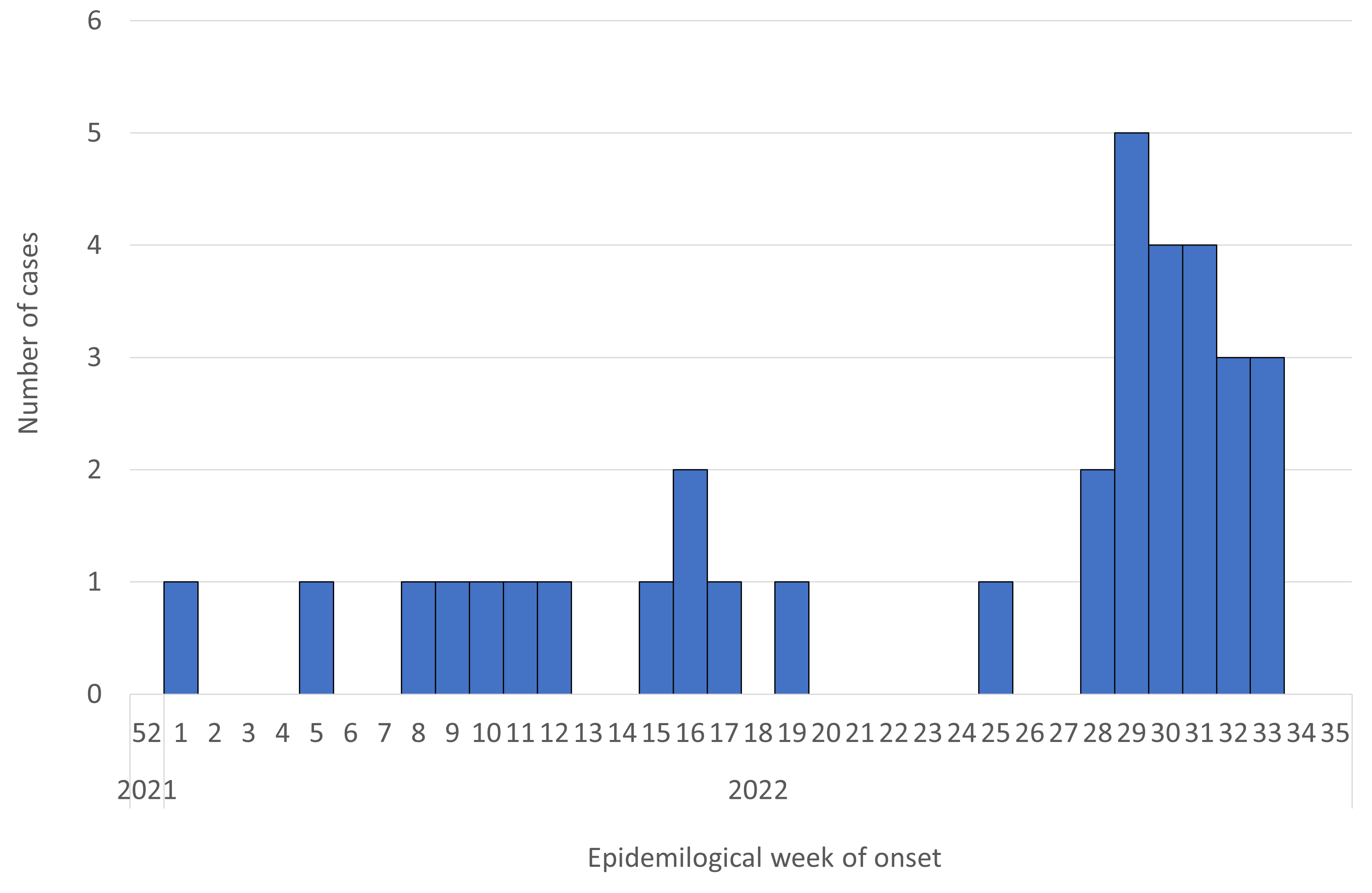
Figure. Reported number of deaths in patients under 20 years of age after SARS-CoV-2 infection (n=34*; date of onset or admission date from January 1, 2022 [week 52, 2021] to August 31, 2022 [week 35, 2022]) (as of August 31, 2022**)
* Seven cases were excluded for unknown date of onset.
** Case numbers in late August may not reflect the actual number of cases due to delayed reporting, so care must be taken in interpreting the data.
〇 Results of the field investigation
Of the 41 cases, we could conduct a field investigation of 32 cases. Among them, 29 cases were considered to be endogenous deaths (death due to other than trauma). The details of these 29 cases are as follows (Table).
Among the 29 cases, eight (28%) patients were <1 year old, six (21%) were 1–4 years old, 12 were 5–11 years old, and three (10%) were 12–19 years old, of whom 16 cases (55%) were in males and 13 cases (45%) were in females. Underlying disease was present in 14 (48%) patients and absent in 15 (52%). As of August 31, 2022, details of underlying disease, including duplicates, showed seven with central nervous system (CNS) abnormalities (50%), two with congenital heart disease (14%), and two with chromosomal abnormalities (14%). Among these 29 patients, 14 (48%) were not eligible for SARS-CoV-2 immunization and 15 (52%) were. Among the 15 patients eligible for SARS-CoV-2 immunization who were 5 years old or older, 13 (87%) were not vaccinated, and two (13%) were vaccinated twice, both of whom were 12 years old or older and whose last vaccination had been more than three months earlier. Moreover, a high number of symptoms or clinical findings on hospital arrival included fever in 23 cases (79%), nausea and/or vomiting in 15 (52%), disturbance of consciousness in 13 (45%), cough in nine (31%), inadequate intake of nutrition in nine (31%), seizure in eight (28%), and dyspnea in seven (24%). The main diseases suspected of causing death in medical institutions included cardiac abnormalities (n=7, 24%: myocarditis, arrhythmia, etc.), CNS abnormalities (n=7, 24%: acute encephalopathy, etc.), respiratory abnormalities (n=3, 10%: pneumonia, bacterial pneumonia, etc.), other diseases (n=6, 21%: multiple organ failure, etc.), and unknown cause of death (n=6, 21%). Several patients with a more rapid disease progression died due to CNS abnormalities such as encephalopathy, etc., and cardiac abnormalities such as myocarditis or arrhythmia. The date of onset was determined in 26 of the 29 cases, and the number of days from onset to death was a median of four days (range: 0–74 days), with eight patients (31%) dying in 0–2 days, 11 dying (42%) in 3–6 days, and seven dying (27%) in 7 days or more.
Of the 29 cases, 14 were thought to have underlying disease, including eight cases (57%) in patients under 5 years old (including four under one year old) and six cases (43%) in patients 6 years old or older. Nine cases (64%) were in males and five cases (36%) were in females. Symptoms or clinical findings on hospital arrival included fever in 11 cases (79%), dyspnea in seven (50%), nausea and/or vomiting in six (43%), cough in five (36%), inadequate intake of nutrition in four (29%), seizure in three (21%), and disturbance of consciousness in three cases (21%). In the medical institutions, the main diseases suspected of causing death were cardiac abnormality (n=3, 21%), respiratory abnormality (n=3, 21%), CNS abnormality (n=2, 14%), other disease (n=3, 21%), and unknown disease (n=3, 21%). Among these 14 cases, date of onset could be obtained in 12, and the number of days from onset to death was a median of four days (range: 1–74 days), with three patients (25%) dying in 0–3 days, seven dying (58%) in 3–6 days, and two dying (17%) in 7 days or more.
Of the 29 cases, 15 were considered to have no underlying disease. These included six cases (40%) in patients under five years old (including four under one year old) and nine cases (60%) in patients over 5 years old. Seven cases (47%) were in males and eight cases (53%) were in females. Symptoms or clinical findings on hospital arrival included fever in 12 cases (80%), disturbance of consciousness in 10 (67%), nausea and/or vomiting in nine (60%), seizure in five (33%), inadequate intake of nutrition in five (33%), cough in four (27%), and no cases (0%) with dyspnea. In the medical institutions, the main diseases suspected of causing death were CNS abnormalities (n=5, 33%), cardiac abnormalities (n=4, 27%), other disease (n=3, 20%), unknown cause of death (n=3, 20%), and respiratory abnormalities (n=0, 0%). Date of onset was obtained in 14 of the 15 cases, and the number of days from onset to death was a median of 4.5 days (range: 0–15 days), with five patients (36%) dying in 0–2 days, four dying (29%) in 3–6 days, and five dying (36%) in 7 days or more.
Table. Characteristics of fatal cases under 20 years of age after SARS-CoV-2 infection (n=29; limited to clearly endogenous deaths occurring only from January 1 to August 31, 2022; as of August 31, 2022)
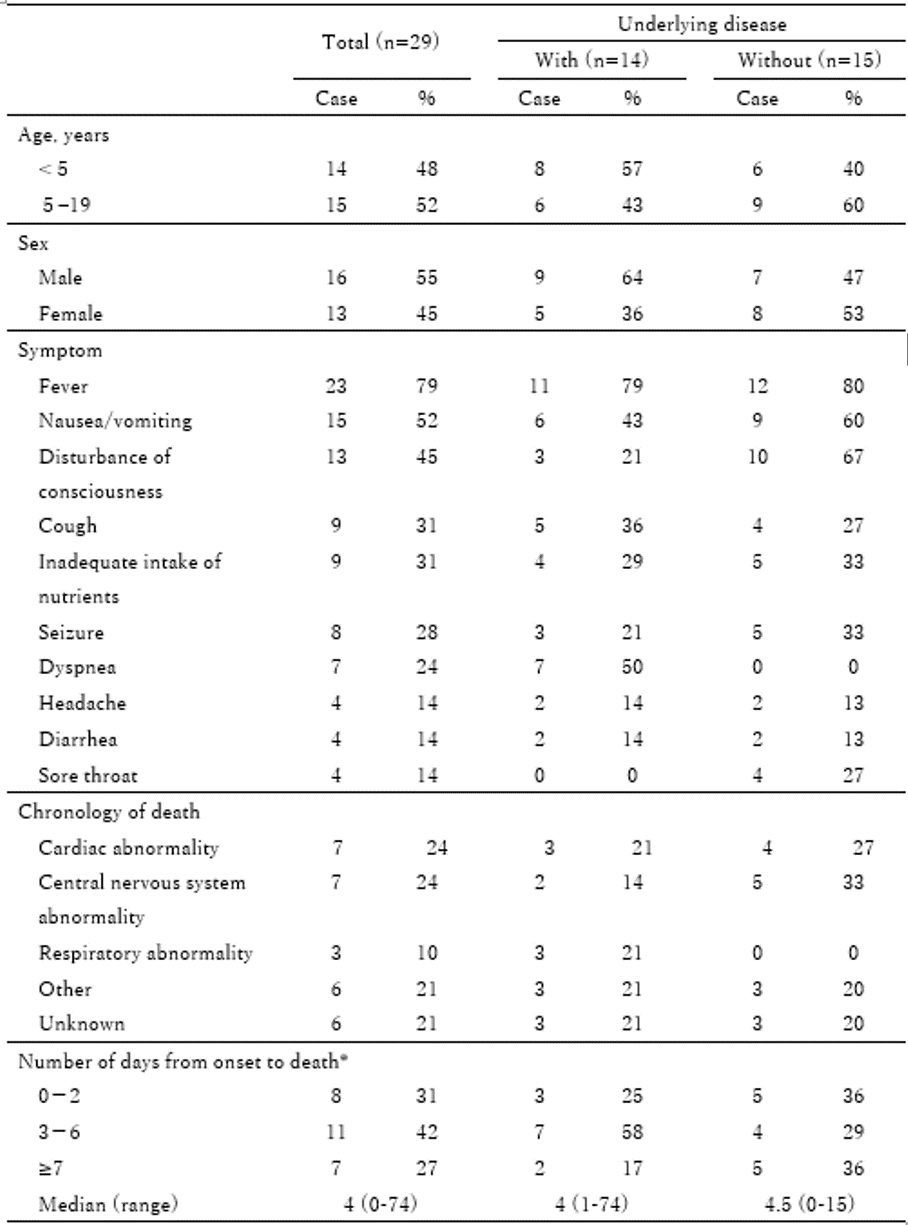
* Three cases whose date of onset or death was uncertain were excluded. Included were 12 cases with underlying disease and 14 cases without underlying disease.
Discussion
As of August 31, 2022, we described the interim report on 41 fatal pediatric cases from January 1 to August 31, 2022.
The number of cases had increased from mid-July 2022. In this field investigation, fatal pediatric cases caused by clearly endogenous factors included those in patients not only with underlying disease but also in patients with no underlying disease. Thus, families and healthcare workers might need to carefully follow the course of symptoms in those after SARS-CoV-2 infection. SARS-CoV-2 immunization was not administered in many of the fatal pediatric cases even though the children were of an approved age for the immunization. Moreover, compared to the registry of Japanese children with COVID-19 done by the Japan Pediatrics Society 2), the symptoms of the fatal pediatric cases in this investigation, except for respiratory symptoms, included a high proportion of nausea and/or vomiting (52%), disturbance of consciousness (45%), inadequate intake of nutrition (31%), and seizure (28%). The severity of COVID-19 is mainly classified only according to respiratory symptoms 3), but our results suggested that pediatric cases should be carefully followed up not only for respiratory symptoms but also for symptoms of CNS abnormalities such as disturbance of consciousness and seizure, vomiting, and inadequate intake of nutrients. The duration from onset to death was under one week in 73% of the patients, and our results further suggested that careful follow-up of the cases was important especially for the first week after onset of the disease.
Limitations and further investigation
This was an interim report as of August 31, 2022, and as the field investigation will continue to collect additional information on the fatal pediatric cases, the report may be revised and/or further information may be added, and we did not examine the causal relationship between SARS-CoV-2 infection and death. Therefore, the results should be carefully interpreted.We plan to continue to investigate fatal pediatric cases in cooperation with the local public health authorities and related academic associations.
Collaborating academic associations
Japan Pediatric Society, The Japanese Society of Intensive Care Medicine, Japanese Association for Acute Medicine.
References
1. Ministry of Health, Labour, and Welfare. Visualizing the data: information on COVID-19 infections. https://covid19.mhlw.go.jp/en/ (accessed on August 19, 2022).
2. Committee on Immunization and Prevention of Infectious Diseases, Japan Pediatric Society. Interim Report on Clinical Course of Domestic-Onset Pediatric Coronavirus Disease 2019 (COVID-19) Cases Using a Database: 3rd Report. Changes in Clinical Symptoms and Severity of Pediatric COVID-19 Cases Associated with the Omicron Epidemic. http://www.jpeds.or.jp/uploads/files/20220328_tyukan_hokoku3.pdf (accessed on August 19, 2022) [in Japanese].
3. Medical Treatment Guidance Review Committee. COVID-19 Treatment guidelines, the 8th Edition. https://www.mhlw.go.jp/content/000967699.pdf (accessed on August 19, 2022) [in Japanese].