Infectious Deseases
Basic Research
Surveillance
Information
- Details
124th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (August 4, 2023)Material 1
Evaluation of the latest Infection Status of COVID-19 Infections
Infection status and situation of the medical care provision system
- The number of new patients has tended to gradually increase since early April, and has continued to increase for 11 consecutive weeks, even after the downgrade to Class 5. Most recently, the number of reports per fixed point nationwide has exceeded 15.
(15.91 per fixed point from 7/24 to 7/30 nationwide, 1.14 compared to the previous week) - The number of new patients by region has increased from the previous week in 42 prefectures. In Okinawa, there has been a decreasing trend from early July.
(17.59 per fixed point from 7/24 to 7/30 in Okinawa, 0.78 compared to the previous week) - The number of new patients by age group is increasing from the previous week nationwide in all age groups except those in their 10s.
- Regarding trends in the occurrence of variants, XBB lineages account for the largest proportion. While the XBB.1.9 lineage tends to level off, the XBB.1.16 and the XBB.2.3 lineages tend to increase, and the XBB.1.5 lineage tends to decrease.
- The numbers of newly hospitalized patients and severe cases are both on an increasing trend and the number of severe cases is increasing, especially since mid-July (It should be noted that recent data are underestimated).
- Regarding the situation of the medical care provision system, although it is not strained anywhere in the country, the number of inpatients is increasing. In Okinawa, the number of inpatients is decreasing.
- In emergency medical care, the number of cases that experience difficulty with emergency transportation tends to continue to increase, both for suspected COVID-19 and non-COVID-19-related cases.
- Regarding the nighttime population, no significant increase was seen anywhere in the country since the downgrade to Class 5.
Future outlook
- Based on previous situations, the number of new patients may continue to increase this summer, which may increase the burden on the medical care provision system.
- It is necessary to pay attention to the impact of the attenuation of immunity that is due to natural infection and vaccination, the increase in the proportion of strains with potential immune escape, and the impact of future increases in contact opportunities, such as the summer vacation, on the infection situation.
Future efforts
- We will continue to pursue obtaining a multi-layered understanding of infection trends, and pay attention to the medical care provision system nationwide.
- For people at high risk of severe illness, such as elderly people and those with underlying diseases, vaccination will continue, and a shift in the medical system will be promoted so that a wide range of medical institutions can handle COVID-19 patients to provide the necessary medical care, even if the infection spreads, in cooperation with local governments and medical personnel.
- We will continue to publicize basic infection control measures, including proper ventilation in particular, wearing of masks in situations where these are effective, and washing of hands, more actively.
- Details
123rd Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (July 7, 2023)Material 1
Evaluation of the Latest Infection Status of COVID-19 Infections
Infection status and situation of the medical care provision system
- The number of new patients has tended to gradually increase since the beginning of April, and has continued to increase for seven consecutive weeks, even after the downgrade to Class 5.
(7.24 per fixed point from 6/26 to 7/2 nationwide, 1.18 compared to the previous week) - The number of new patients by region tended to increase from the previous week in 46 prefectures, and the spread of infection can be seen particularly in Okinawa.
(48.39 per fixed point from 6/26 to 7/2 in Okinawa, 1.23 compared to the previous week) - The number of new patients by age group is increasing nationwide in all age groups from the previous week.
- Regarding trends in the occurrence of variants, XBB lineages account for most of them, and in particular, the XBB.1.16 lineage tends to increase, the XBB.1.5 lineage tends to decrease, and the XBB.1.9 lineage remains flat.
- The numbers of newly hospitalized patients and severe cases are both on an increasing trend (It should be noted that recent data are underestimated).
- Regarding the situation of the medical care provision system, although it is not strained nationwide, the burden on the healthcare systems is increasing in Okinawa because of an increase in the number of inpatients and the occurrence of in-hospital clusters.
- In emergency medical care, the number of cases of difficult emergency transportation remains almost flat for both suspected COVID-19 and non-COVID-19 cases.
- Regarding the nighttime population, no significant increase was seen nationwide since the downgrade to Class 5.
Future outlook
- Based on the past situation, it is possible that the number of new patients will continue to increase, and that infection will spread to a certain extent during the summer. The spread of infection may also increase the burden on the medical care provision system.
- It is necessary to pay attention to the impact of the attenuation of immunity that is due to natural infection and vaccination, the increase in the proportion of strains with potential immune escape, and the impact of future increases in contact opportunities on the infection situation.
Future efforts
- Pursuit of a multi-layered understanding of infection trends as well as close cooperation, particularly with Okinawa, where the infection is spreading, will continue.
- For people at high risk of severe illness, such as elderly people and those with underlying diseases, vaccination will continue, and a shift in the medical system will be promoted so that a wide range of medical institutions can handle COVID-19 patients to provide the necessary medical care, even if the infection spreads, in cooperation with local governments and medical personnel.
- We will continue to publicize basic infection control measures such as the washing of hands, ventilation, and wearing of masks in situations where these are effective, more actively.
- Details
122nd Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (June 16, 2023)Material 1
Evaluation of the Latest Infection Status of COVID-19 Infections
Infection status and situation of the medical care provision system
- The number of new patients has tended to gradually increase since the beginning of April, and has continued to increase for four consecutive weeks even after the downgrade to Class 5.
(5.11 per fixed point from 6/5 to 6/11, 1.12 compared to the previous week) - The number of new patients by region tended to increase from the previous week in 36 prefectures, and a tendency for infection to spread can be seen in Okinawa.
(18.41 per fixed point from 6/5 to 6/11, 1.17 compared to the previous week) - The number of new patients by age group is increasing nationwide from the previous week, except for those aged 80 and over.
- Regarding trends in the occurrence of variants, XBB lineages account for most of them, and in particular, the XBB.1.16 lineage tends to increase, the XBB.1.5 lineage tends to decrease, and the XBB.1.9 lineage remains flat.
- The numbers of newly hospitalized patients and severe cases are both on an increasing trend (It should be noted that recent data are underestimated).
- Regarding the situation of the medical care provision system, although it is not strained nationwide, the situation in Okinawa demands attention.
- In emergency medical care, the number of cases of difficult emergency transportation has increased recently for both suspected COVID-19 and suspected non-COVID-19 cases.
- Regarding the nighttime population, no significant increase has been seen nationwide since the downgrade to Class 5.
Future outlook
- Based on the past situation, it is possible that the number of new patients will continue to increase, and that infection will spread to a certain extent during the summer. The spread of infection may also increase the burden on the medical care provision system.
- It is necessary to pay attention to the impact of the attenuation of immunity that is due to natural infection and vaccination, the increase in the proportion of strains with potential immune escape, and the impact of future increases in contact opportunities on the infection situation.
Future efforts
- Pursuit of a multi-layered understanding of infection trends will continue, paying particular attention to medical care provision systems in regions where the number of infected people is still increasing.
- For people at high risk of severe illness, such as the elderly and those with underlying diseases, vaccination will continue to proceed, as well as shift to a medical system will promote so that a wide range of medical institutions will handle COVID-19 patients in order to provide necessary medical care even if the infection spreads, in cooperation with local governments and medical personnel.
- Basic infection control measures such as washing hands, ventilation, and wearing masks in effective situations will be promoted.
- Details
121st Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (April 19, 2023)Material 1
Evaluation of the latest infection status, etc.
Overview of the infection status, etc.
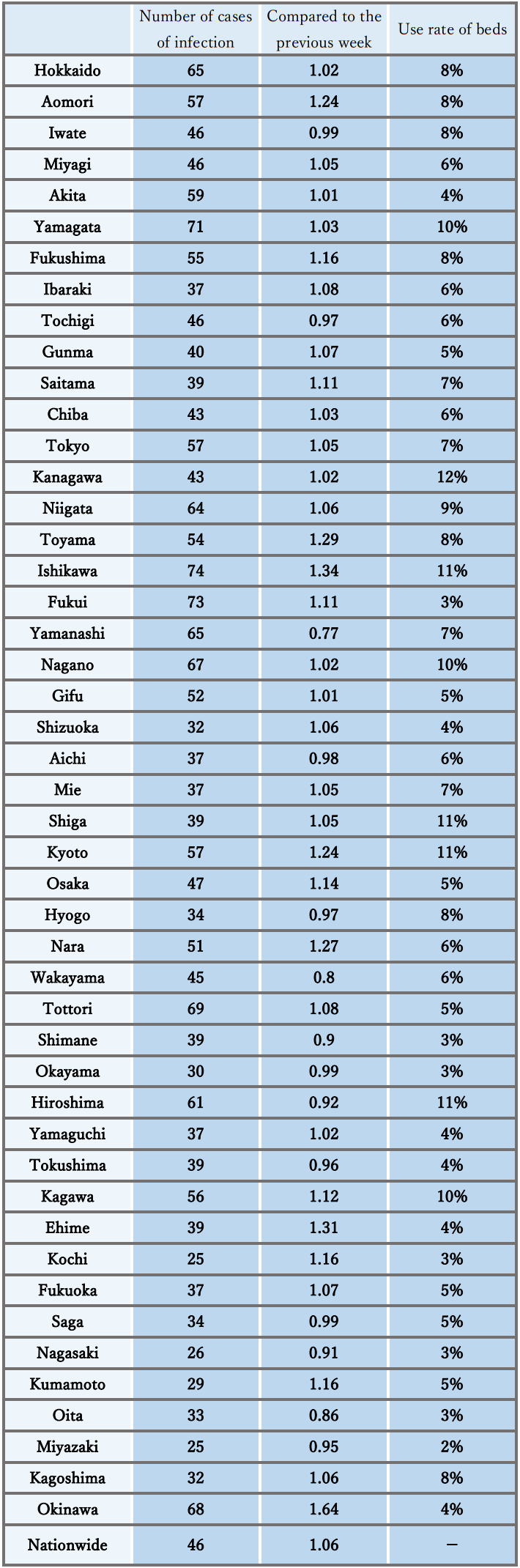
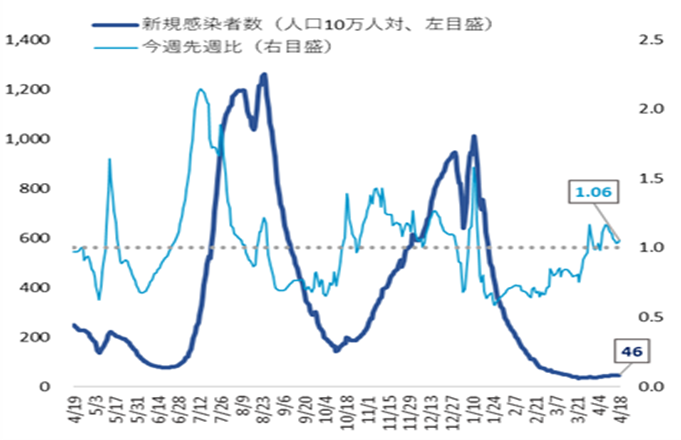
- The number of new cases of infection nationwide was approximately 46 per 100,000 of the population in the last week, showing a gradually increasing trend with a ratio of this week to last week of 1.06.
It is necessary to pay attention to the impact of increased opportunities for contact, attenuation of immunity, and replacement by variant strains on the infection status. - The numbers of severe patients and deaths remain flat, and the use rate of beds is at a low level nationwide.
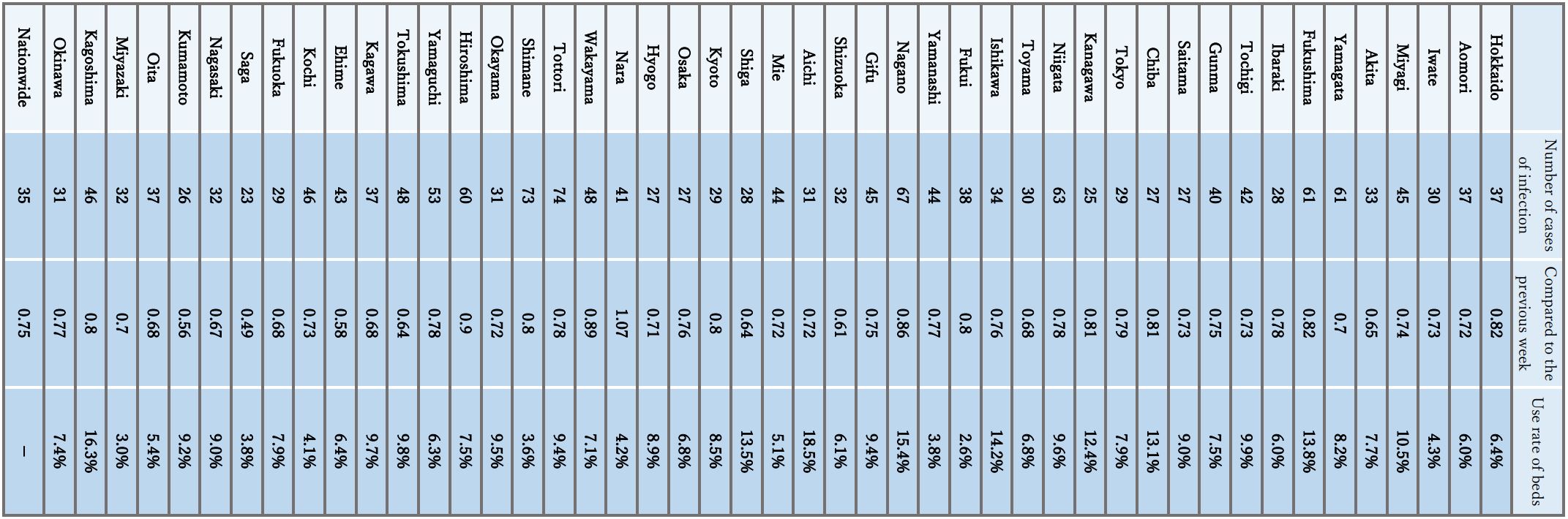
Reference: Local trend
* The number of new cases of infection is an approximate figure per 100,000 of the population, as the total for the current week, which is the reported number in HER-SYS as of Apr. 18 at 00:00 AM (the same time point is used for the ratio to the previous week), and the use rate of beds is the secured bed use rate as of the time of the announcement on Apr. 14.
Infection status and future outlook
Infection status
- The number of new cases of infection has gradually been increasing after a nationwide halt. On the other hand, the level continues to be lower than before the spread of infection in the summer last year (2022).
- Regarding the number of new cases of infection by region, in Hokkaido, the Hokuriku-Koshinetsu region, and Okinawa, the number per population is higher than the national average. Meanwhile, in the Tokai, Shikoku, and Kyushu regions, the number is lower than the average. In addition, the number of cases of mass infection in facilities for elderly people and medical institutions has leveled off.
- Seen by age group, the number of new cases of infection has recently increased in teens and younger people nationwide, although the number has also increased in people in their 20s in some large cities such as Tokyo and Osaka.
- The numbers of severe patients and deaths remain flat nationwide. With the spread of infection this winter, the proportion of elderly patients in their 80s and older among newly infected patients tended to increase, compared to that during the spread of infection in the summer last year (2022).
- As the reports of deaths among children since January 2022 suggest, attention must be paid to the occurrence of severe cases and deaths as well as the number of hospitalized children associated with an increase in the number of infected children.
- Regarding seasonal influenza, at the time of the announcement last weekend, the weekly number of reports per fixed-point medical institution was decreasing nationwide, and is far below the advisory level.
Future outlook
- Attention should be paid to the future infection status because the number of new cases of infection may remain flat or continue to show a gradually increasing trend nationwide, although it may differ among regions. It is also necessary to pay attention to the future impact of increased opportunities for contact, the attenuation of immunity, and an increase in the proportion of strains that can escape the immune system, on the infection status.
- In light of the situation the past 2 years, it is considered that the infection will spread after the consecutive holidays in May, that it will decrease once and then spread again in the summer.
- Although seasonal influenza is still at the advisory level in some regions, it is expected to decrease further based on past trends.
Factors that increase and suppress infection
- [Immunity as a result of vaccination and infection]
With the promotion of vaccination and natural infection, it is considered that the proportion of immune carriers against the Omicron variant (BA.5 and BQ1.1), which has shown an increase in each age group, will decrease over time in the future.
- [Contact status]
There are many regions where the nighttime population is currently decreasing compared to the level at the start of the new fiscal year. In the future, however, opportunities for contact is expected to increase due to the consecutive holidays in May.
- [Epidemic strain]
In Japan, the BA.5 lineage, including the BQ.1 lineage, was mainstream, but its proportion has tended to decrease since around March. On the other hand, the proportions of the XBB.1.5 lineage, which is frequently reported in the United States, the XBB.1.9 lineage, which is frequently reported in Europe, and the XBB lineage including the XBB.1.16 lineage, which is frequently reported in India, are on the rise. Since the number of registered variant strains is decreasing as the number of infected people in Japan decreases, caution is required when considering the proportion of variant strains.
- [Climate/Seasonal Factors]
With the temperature rising now, the climate conditions will facilitate ventilation. It is thought that a reduction of the amount of time spent indoors has a certain effect on suppressing infection; however, it should be noted that the infection may spread during this period.
Situation of the medical care provision system
- The use rate of beds is at a low level below 10% in most regions. The use rate of beds for severe patients is also low nationwide.
- The number of patients receiving treatment in nursing care facilities has continued to decrease.
- Regarding emergency medical care, the number of cases where emergency transportation is difficult remains flat nationwide, but attention should continuously be paid to the future trend of the number of cases where emergency transportation is difficult and securing of a system to provide emergency medical care.
Measures to be taken
Basic concepts
- Unless we face special circumstances such as the emergence of a variant with a pathogenicity greatly different from that of the Omicron variant, COVID-19 shall be positioned as a Class V Infectious Disease instead of a Novel Influenza Infection, etc. under the Infectious Disease Act from May 8 this year (2023). In association with this, the government decided on March 10 this year to make necessary revisions to various policies and measures that have been taken, such as the medical care system, response to facilities for the elderly, and public financial support for patients.
- Meanwhile, it is necessary to continue efforts to strengthen and focus the healthcare system to provide appropriate medical care for elderly people and those at high risk of aggravation, even with limited medical resources. Each citizen will be asked to take voluntary actions to prevent infection to protect those at high risk of aggravation, such as elderly people, and to ensure regular medical care.
- 1. Further promotion of vaccination
- As for the “vaccine for the Omicron variant," vaccination of all persons aged 5 and older who have completed the first vaccination should proceed.
- All eligible persons who wish to receive vaccination will be encouraged to receive the vaccine for the Omicron variant.
- Those who have not received vaccination will be encouraged to consider getting the initial vaccination as soon as possible.
- For children (aged 5 to 11 years), the initial vaccination and additional vaccination with the vaccine for the Omicron variant will be promoted. For children (aged 6 months to 4 years), the initial vaccination will be promoted.
- Vaccination in FY 2023 will be promoted (vaccination will be given to all eligible persons aged 5 years and older in autumn and winter, and vaccination will be given to elderly people and those at high risk of aggravation in spring and summer, without waiting until autumn or winter).
- 2. Use of tests
- The national and local governments are required to secure a system that enables testing, and should utilize testing.
- Perform frequent tests (about 2 or 3 times a week for facility workers) for workers at facilities for elderly people.
- Promote the establishment of a system for fever outpatients, whereby patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Promote the utilization of antigen qualitative test kits, which have been switched to OTC and are sold on the Internet.
- 3. Effective ventilation
- It is necessary to publicize and recommend effective indoor ventilation methods (such as how to create airflow considering aerosols, the installation of partitions that do not block airflow, etc.).
- 4. Securing a medical care provision system
- With support of the national government, local governments continue to take measures to avoid overcrowding of hospital beds, fever clinics, etc.
- Make appropriate adjustments so that patients who need hospital treatment can be hospitalized preferentially (securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule). Implement frequent examinations at facilities for elderly people and others. Further strengthen medical support during normal times.
- Local residents should be informed that they should refrain from visiting emergency outpatient units only to receive a precautionary examination if they do not have symptoms, for example, taking the actual situation in the region into consideration, so that nobody is prevented from receiving treatment. To respond to concerns and questions when a patient’s physical condition deteriorates, the telephone consultation service by healthcare professionals should be thoroughly publicized, and this service should also be strengthened.
- In response to the government's decision on March 10 this year, with the change in positioning as a Class V Infectious Disease, encourage medical facilities that have been responding to the new coronavirus infection to continue to respond, and start efforts to encourage new medical facilities to participate.
- Maintenance and expansion of responding medical institutions through review of infection control measures, support for maintenance of facilities, clarification of the obligation to provide treatment, and dissemination of easy-to-understand educational materials on infection control and medical treatment policies
- In each prefecture, until the expansion of infection in the next winter a transition plan up to the end of September will be formulated in April, with contents such as the acceptance of patients with mild disease by new medical institutions, and the coordination of hospitalization among medical institutions.
- 5. Response to simultaneous epidemics of COVID-19 and seasonal influenza
- The following efforts should be promoted according to the actual situation in each region: fever outpatient clinics, telephone consultations/telemedicine, health follow-up centers, self-test kits, consultation system, and emergency medical care. Smooth supply of medications including oral drugs prescribed after confirmation of the indication by physicians will be promoted. Pharmacies, etc. will be asked to use the consultation service of the Ministry of Health, Labour and Welfare regarding antipyretic analgesics, etc.
- The prefectures will work to strengthen and prioritize the health care system based on plans to establish systems such as strengthening of outpatient medical care systems in accordance with the actual conditions in each region.
- It is necessary to provide information and send appropriate messages to the public depending on the infection status. People at low risk of aggravation will be encouraged to use a self-test kit or local follow-up center.
- People will be advised to do the following: check the “guide for ambulance services” in preparation for an acute illness or injury, consult a family doctor when hesitant to call an ambulance, use a telephone consultation service such as #7119, and call an ambulance without hesitation if necessary.
- 6. Surveillance and risk assessment, etc.
- After the position of COVID-19 under the Infectious Disease Act is changed on May 8 this year (2023), preparations will be made in cooperation with local governments to perform a stratified analysis through continued seroepidemiologic surveys, sewage surveillance studies, etc. to grasp and publish data such as the numbers of infected patients, hospitalized patients, and deaths. Monitoring of the trends of variant strains will also be continued through genome surveillance.
- Regarding the risk assessment of COVID-19, it is necessary to continue evaluation of the pathogenicity, infectivity, mutations, etc.
- 7. Quarantine measures
- Regarding temporary measures for people entering from China after December 30th last year, sample tests at entry which have been conducted for some people entering Japan since March 1 this year will be continued. From April 5th this year, instead of submission of a negative certificate, those who enter from China by mainland flight will be required to submit either a negative certificate or a certificate of vaccination (three times), considering the situation of infections in Japan and overseas, knowledge obtained through temporary measures, and the status of quarantine measures in G7 countries.
- Along with the end of quarantine measures scheduled for May 8 this year (2023), Infection Genome Surveillance (provisional name) will start on the same day to monitor the influx of new infectious diseases, even in ordinary times.
- 8. Re-inspection and implementation of basic infection control measures
Everyone must take the following basic precautions from the perspective of being aware of the epidemic of infectious disease in the community, protecting ourselves from infectious disease, and protecting people close to us as well as society from infectious disease, especially the elderly.
- If feeling unwell or having symptoms, do not overdo it, and be treated at home or see a doctor.
- Hand hygiene such as hand washing as a daily habit
- Wearing a mask and practicing cough etiquette according to the situation
- Understanding and practicing lifestyle habits such as moderate exercise and diet
- Enforcement of ventilation, and avoiding crowded places, close contact, and closed spaces (the 3 Cs)
- Make efforts such as promoting the use of telework in the workplace.
- From May 8 this year, the government will not uniformly request the use of basic infection control measures but will respect the independent choice of individuals and leave it to their judgment.
- Concerning the period of home care for people who test positive, they should monitor their own physical condition by such means as checking their body temperature and take thorough infection control measures when going out. They are also requested to avoid contact with people who are at risk of severe disease, such as elderly people. From May 8 this year (2023), it will be recommended that they refrain from going out for 5 days after the onset of disease and 24 hours after the alleviation of symptoms. It will also be recommended that they wear a mask and avoid contact with high-risk people until 10 days have passed from then.
- To allow the minimum necessary outings, such as shopping for groceries, after 24 hours have passed since symptoms have subsided or when there are no symptoms, it is necessary to take voluntary actions to prevent infection, such as wearing a mask when going out, keeping contact with other people at the minimum period of time possible, and not using public transportation.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is also considered to have occurred via droplets adhering to mucosa, aerosol inhalation, contact infection, etc.
- [Severity, etc.]
It has been shown that infection with the Omicron variant may present a relatively lower risk of hospitalization or aggravation than with the Delta variant. To evaluate COVID-19, including the Omicron variant, it is necessary to assess not only the severity as a disease but also the transmissibility and the impact on medical care and society.
Concerning the death toll during the spread of infection from the end of 2021, it has been reported that COVID-19 was not the direct cause of death in quite a number of cases, compared to that during the spread of infection in the summer of 2021; for example, there were deaths due to the worsening of underlying diseases after infection with the novel coronavirus in elderly people who had been living in a facility for elderly people since before the infection. There were many cases of serious respiratory failure due to typical viral pneumonia caused by the novel coronavirus infection from the beginning of the novel coronavirus outbreak until the Delta variant epidemic. However, during the Omicron variant epidemic, it was reported that other diseases than pneumonia became the main cause of death, such as the exacerbation of underlying disease that had been present before hospitalization and the onset of other complications during hospitalization.
During the spread of infection last summer, a decrease in the rate of severe cases and an increase in the proportion of elderly people among hospitalized patients were seen, as had been seen previously, compared to the spread of infection in the summer of 2021. In addition, compared to the situation during the spread of infection since the end of 2021, the rates of mechanical ventilation/nasal high flow use and steroid prescription among the number of deaths associated with the spread of infection was lower during the summer of 2022.
Among the fatal cases of infected children who died of endogenous factors, there were some cases without any underlying diseases. Reports on the results of on-site investigations have stated that it is necessary to pay attention to neurological symptoms such as convulsions and disturbance of consciousness as well as systemic symptoms such as vomiting and poor oral intake besides respiratory symptoms.
Among the deaths that occurred at home in July and August last year, approximately 80% of the patients were 70 years and older, which is similar to the trend of all deaths during the same period. It suggests that there were also many deaths caused by factors other than COVID-19. Regarding the situation of handling known coronavirus-positive corpses, the number of cases reported monthly was the highest in December last year (2022). The proportion of deaths due to COVID-19 was approximately 30% of all deaths.
- [Virus shedding period]
Japanese data suggest that infectious viruses are expelled in the period from 2 days before the onset of symptoms to 7-10 days after the onset, and that the mean amount of expelled infectious viruses is very high in the first 3 days after the onset of symptoms and greatly decreases to one-twentieth to one-fiftieth the amount on the day of onset after 5 days have passed, approaching the detection limit, although there are individual differences.
- [Vaccine effects]
Concerning conventional vaccines, the infection and disease onset prevention effects of the first vaccination against the Omicron variant have been markedly reduced. The hospitalization-preventing effect is reported maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing, disease onset-preventing and hospitalization-preventing effects against infection with the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Concerning the vaccine for the Omicron variant (BA.4-5), it has been reported that the preventive effect against disease onset was observed within 0 to 2 months (median 1 month) after vaccination.
- [Sublineages of the Omicron variant]
The proportion of the BA.5 lineage, which was the mainstream worldwide, is declining, and on the other hand, the proportion of the XBB lineage (a recombinant of the BJ.1 lineage [a sublineage of the BA.2.10 lineage] and the BM.1.1.1 lineage [a sublineage of the BA.2.75.3 lineage]), including the XBB.1.5 lineage, is increasing currently. The proportion of the XBB.1.5 lineage, the XBB.1.9 lineage, and the XBB.1.16 lineage (all of them include sublineages) is increasing in the United States, Europe, and India, respectively. The severity of disease caused by the XBB.1.5 lineage is not higher than that caused by the BQ.1 lineage, but its clinical picture and epidemiological findings are otherwise insufficient. The clinical picture and epidemiological findings are also insufficient regarding the XBB.1.9 lineage and the XBB.1.16 lineage. It is therefore necessary to continue collecting and analyzing data on overseas situations and to continue monitoring through genome surveillance. Caution should be exercised when considering the proportion of variant strains because the number of registered variant strains is decreasing as the number of infected people decreases worldwide.
Figures (Number of new infections reported etc.) (PDF)
- Details
Updated April 21, 2023 at 9:00 am
National Institute of Infectious Diseases, Japan
*This is a provisional translation of the summary of the report entitled "kansen-denpasei no zoukaya kougenseino henkaga kenensareru SARS-CoV-2 no henikabunituite (dai27hou) (https://www.niid.go.jp/niid/ja/2019-ncov/2551-cepr/11879-sars-cov-2-27.html)". In the case of any dispute over translation, Japanese text prevails.
Overview of SARS-CoV-2 variants
The Omicron variant, along with its B.1.1.529 lineage and descendant sub-lineages, remains dominant globally among SARS-CoV-2 variants, and there have been no significant changes in epidemiological trends since the No. 26 report. Several sub-variants and recombinant omicron variants have been reported. The WHO has classified XBB.1.5 as a currently circulating variant of interest (VOI) and BA.2.75, CH.1.1, BQ.1, XBB, XBB.1.16, XBB.1.9.1, and XBF as currently circulating variants under monitoring (VUMs) since April 12, 2023.
However, there were no significant changes in viral characteristics, such as severity and infectivity/transmissibility, apart from an increase in the number of infected cases and the possibility of immune escape between subvariants. Thus, NIID continues to classify the subvariants as before. It is important to continue monitoring and collecting information on subvariant outbreaks through genomic analysis in the country and quarantine.
According to the WHO weekly epidemiological updates on COVID-19 (April 13, 2022), 47.9% of XBB.1.5 sequences, 7.6% of XBB.1.9.1 and 17.6% of the other XBB variant (excluding XBB.1.5, XBB.1.16, and XBB.1.9.1) were reported in the 12th week of 2023 (March 20-26, 2023).
In Japan, BA.5 replaced BA.2 around July 2022, and the relative sequence prevalence among circulating variants has been dominated by BA.5, followed by an increasing proportion of BQ.1 (a sub-lineage of the BA.5.3 lineage) and BA.2.75 (a sub-lineage of the BA.2 lineage) since October 2022. The proportion of XBB variants has increased since January 2023.
Some subvariants, such as BQ.1 and XBB, exhibit characteristic mutations in the spike protein that allow the virus to evade neutralizing antibodies generated through vaccination or previous infection and may have a growth advantage. Some subvariants, such as XBB.1.5 in North America, XBB.1.9 in Europe, and XBB.1.16 in India, may have a growth advantage over existing sub-lineages in certain regions. However, there is no evidence that these variants spread more rapidly than other variants.
Omicron sub-variants have emerged with specific characteristics that primarily contribute to immune escape. There were no significant differences compared with the other variants, except for this feature. Global immunity and several public health interventions in each country have resulted in less of an impact of the variant-specific nature on epidemic dynamics. Regular monitoring of variant prevalence and changes in variant-specific features, including pathogenicity, virulence, transmissibility, vaccine and antiviral resistance, and clinical presentation, is crucial for determining appropriate interventions and rapid risk assessment for each variant.
- Details
120th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (April 5, 2023)Material 1
Evaluation of the latest infection status, etc.
Overview of the infection status, etc.
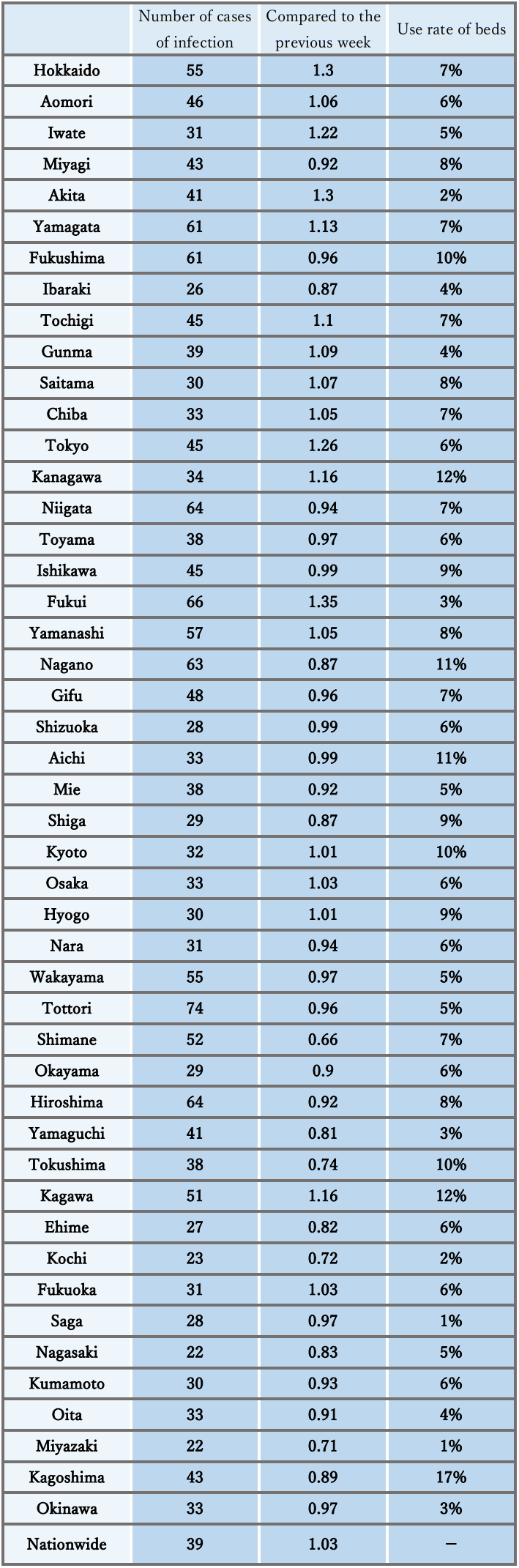
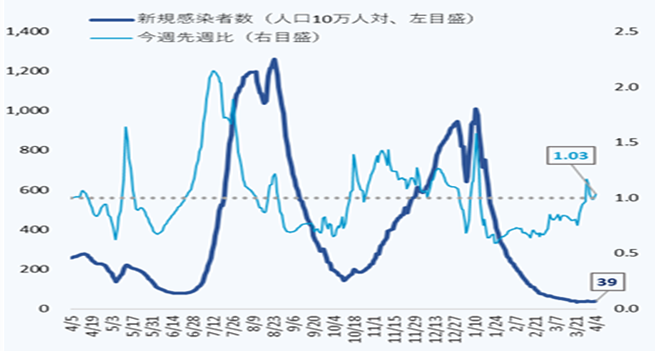
- The number of new cases of infection nationwide was approximately 39 per 100,000 of the population in the last week, a ratio to the previous week of 1.03, and it has stopped declining nationwide, with regions that have seen an increase.
It is necessary to pay attention to situations where the risk of infection increases at the change of the fiscal year, and the impact on the infection situation of the attenuation of immunity and replacement by variant strains. - The use rate of beds has been decreasing nationwide, and the numbers of severe cases and deaths have also continued to decrease.
Reference: Local trend
* The number of new cases of infection is an approximate figure per 100,000 of the population, as the total for the current week, which is the reported number in HER-SYS as of Apr. 4, 00:00 AM (the same time point is used for the ratio to the previous week), and the use rate of beds is the secured bed use rate as of the time of announcement on Mar. 31.
Infection status and future outlook
Infection status
- The number of new cases of infection has stopped decreasing nationwide, and there are currently many regions that are increasing, including large cities. On the other hand, the level continues to be lower than before the spread of infection in summer last year.
- Regarding the number of new cases of infection by region, in Hokkaido and the Hokuriku-Koshinetsu region the number per population is higher than the national average. Meanwhile, in the Kinki and Kyushu regions, the number is lower than the average. In addition, there is a continuous decreasing trend in mass infections in facilities for elderly people and medical institutions.
- Although the number of new infections nationwide by age group continues to decline on average for all age groups, there are some age groups who are increasing, such as those in their 20s.
- The numbers of severe cases and deaths continue to show a downward trend nationwide. With the spread of infection this winter, the proportion of elderly patients in their 80s and older among newly infected patients tended to increase, compared to that during the spread of infection in the summer last year.
- As the reports of deaths among children since January 2022 suggest, attention must be paid to the occurrence of severe cases and deaths as well as the number of hospitalized children associated with an increase in the number of infected children.
- Regarding seasonal influenza, at the time of the announcement last weekend, the weekly number of reports per fixed-point medical institution was decreasing nationwide, and is below the advisory level.
Future outlook
- Regarding the future infection situation, it is necessary to keep an eye on the current trend of increase in the number of infected people in urban areas, especially increases among people in their 20s, as the number of infected people may increase in the future. It is possible that the number of new cases of infection will continue to be flat nationwide based on the epi curve and the short-term forecast nationwide and in large cities, although there are regional differences and uncertainty, and some areas such as Tokyo are expected to show an increasing trend. It is necessary to pay attention to future situations where the risk of infection increases at the change of the fiscal year, and the impact on the infection situation of the attenuation of immunity and increase in the proportion of strains with the ability to escape the immune system.
- Although seasonal influenza is still at the advisory level in some regions, it is expected to decrease further based on past trends.
Factors that increase and suppress infection
- [Immunity as a result of vaccination and infection]
With the promotion of vaccination and natural infection, the proportion of immune carriers against the Omicron variant (BA.5 and BQ1.1), which has shown an increase in each age group, is thought to decrease over time in the future.
- [Contact status]
The nighttime population is currently decreasing in some regions, while it is increasing in other areas such as the Tokyo metropolitan area. The number of opportunities for contact is expected to continue to increase due to spring vacation and the new fiscal year.
- [Epidemic strain]
In Japan, the BA.5 lineage was mainstream, but its proportion has tended to decrease since around March. The proportions of the XBB lineage, including the XBB1.5 lineage which is frequently reported in Europe and the United States, and the BN.1.3 lineage, which is a sub-lineage of the BA2.75 lineage, are on an increasing trend. On the other hand, the BQ.1 lineage, which was increasing in number and proportion in Japan, has been decreasing since peaking in early January. However, since the number of registered mutant strains is decreasing as the number of infected people in Japan decreases, caution is required when considering the proportion of mutant strains.
- [Climate/Seasonal Factors]
With the temperature rising now, the climate conditions will facilitate ventilation. It is thought that a reduction of the amount of time spent indoors has a certain effect on suppressing infection; however, it should be noted that the infection may spread during this period.
Situation of the medical care provision system
- The use rate of beds shows a decreasing trend nationwide and is at a low level below 20% in all regions. The use rate of beds for severe cases is also low nationwide.
- The number of patients receiving treatment in nursing care facilities has continued to decrease.
- Regarding emergency medical care, the number of cases of difficult emergency transport has been decreasing nationwide, but attention should continuously be paid to the future trend of the number of cases having difficulty with emergency transportation and securing a system to provide emergency medical care
Measures to be taken
Basic concepts
- Unless we face special circumstances such as the emergence of a variant with a pathogenicity greatly different from that of the Omicron variant, COVID-19 shall be positioned as a Class V Infectious Disease instead of a Novel Influenza Infection, etc. under the Infectious Disease Act from May 8 this year (2023). In association with this, the government decided on March 10 this year to make necessary revisions to various policies and measures that have been taken, such as the medical care system, response to facilities for the elderly, and public financial support for patients.
- Meanwhile, it is necessary to continue efforts to strengthen and focus the healthcare system to provide appropriate medical care for elderly people and those at high risk of aggravation, even with limited medical resources.
- Each citizen will be asked to take voluntary actions to prevent infection to protect those at high risk of aggravation, such as elderly people, and to ensure regular medical care.
- 1. Further promotion of vaccination
- As for the “vaccine for the Omicron variant," vaccination of all persons aged 5 and older who have completed the first vaccination should proceed.
- All eligible persons who wish to receive vaccination will be encouraged to receive the vaccine for the Omicron variant.
- Those who have not received vaccination will be encouraged to consider getting the initial vaccination as soon as possible.
- For children (aged 5 to 11 years), the initial vaccination and additional vaccination with the vaccine for the Omicron variant will be promoted. For children (aged 6 months to 4 years), the initial vaccination will be promoted.
- Vaccination in FY 2023 will be promoted (vaccination will be given to all eligible persons aged 5 years and older in autumn and winter, and vaccination will be given to elderly people and those at high risk of aggravation in spring and summer, without waiting until autumn or winter).
- 2. Use of tests
- The national and local governments are required to secure a system that enables testing, and should utilize testing.
- Perform frequent tests (about 2 or 3 times a week for facility workers) for workers at facilities for elderly people.
- Promote the establishment of a system for fever outpatients, whereby patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Promote the utilization of antigen qualitative test kits, which have been switched to OTC and are sold on the Internet.
- 3. Securing a medical care provision system
With support of the national government, local governments continue to take measures to avoid overcrowding of hospital beds, fever clinics, etc.
- Make appropriate adjustments so that patients who need hospital treatment can be hospitalized preferentially (securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule). Implement frequent examinations at facilities for elderly people and others. Further strengthen medical support during normal times.
- Local residents should be informed that they should refrain from visiting emergency outpatient units only to receive a precautionary examination if they do not have symptoms, for example, taking the actual situation in the region into consideration, so that nobody is prevented from receiving treatment. To respond to concerns and questions when a patient’s physical condition deteriorates, the telephone consultation service by healthcare professionals should be thoroughly publicized, and this service should also be strengthened.
- In response to the government's decision on March 10 this year, with the change in positioning as a Class V Infectious Disease, encourage medical facilities that have been responding to the new coronavirus infection to continue to respond, and start efforts to encourage new medical facilities to participate.
- Maintenance and expansion of responding medical institutions through review of infection control measures, support for maintenance of facilities, clarification of the obligation to provide treatment, and dissemination of easy-to-understand educational materials on infection control and medical treatment policies
- In each prefecture, until the expansion of infection in the next winter a transition plan up to the end of September will be formulated in April, with contents such as the acceptance of patients with mild disease by new medical institutions, and the coordination of hospitalization among medical institutions.
- 4. Response to simultaneous epidemics of COVID-19 and seasonal influenza
- The following efforts should be promoted according to the actual situation in each region: fever outpatient clinics, telephone consultations/telemedicine, health follow-up centers, self-test kits, consultation system, and emergency medical care.
Smooth supply of medications including oral drugs prescribed after confirmation of the indication by physicians will be promoted. Pharmacies, etc. will be asked to use the consultation service of the Ministry of Health, Labour and Welfare when it is difficult to obtain antipyretic analgesics. - The prefectures will work to strengthen and prioritize the health care system based on plans to establish systems such as strengthening of outpatient medical care systems in accordance with the actual conditions in each region.
- It is necessary to provide information and send appropriate messages to the public depending on the infection status. People at low risk of aggravation will be encouraged to use a self-test kit or local follow-up center.
- People will be advised to do the following: check the “guide for ambulance services” in preparation for an acute illness or injury, consult a family doctor when hesitant to call an ambulance, use a telephone consultation service such as #7119, and call an ambulance without hesitation if necessary.
- The following efforts should be promoted according to the actual situation in each region: fever outpatient clinics, telephone consultations/telemedicine, health follow-up centers, self-test kits, consultation system, and emergency medical care.
- 5. Surveillance and risk assessment, etc.
- It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status. It is also necessary to continue monitoring of the trends of variants through genomic surveillance.
- Regarding the risk assessment of COVID-19, it is necessary to continue evaluation of the pathogenicity, infectivity, mutations, etc.
- 6. Quarantine measures
- Regarding temporary measures for people entering from China after December 30th last year, sample tests at entry which have been conducted for some people entering Japan since March 1 this year will be continued. From April 5th this year, instead of submission of a negative certificate, those who enter from China by mainland flight will be required to submit either a negative certificate or a certificate of vaccination (three times), considering the situation of infections in Japan and overseas, knowledge obtained through temporary measures, and the status of quarantine measures in G7 countries.
- Along with the end of quarantine measures scheduled for May 8, we will start Infection Genome Surveillance (provisional name) will start on the same day in order to monitor the influx of new infectious diseases even in ordinary times.
- 7. Effective ventilation
- It is necessary to publicize and recommend effective ventilation methods to prevent insufficient indoor ventilation (such as how to create airflow considering aerosols, installation of partitions that do not block airflow).
- 8. Re-inspection and implementation of basic infection control measures
Everyone must take the following basic precautions from the perspective of being aware of the epidemic of infectious disease in the community, protecting ourselves from infectious disease, and protecting people close to us as well as society from infectious disease, especially the elderly.
- If feeling unwell or having symptoms, do not overdo it, and be treated at home or see a doctor.
- Hand hygiene such as hand washing as a daily habit
- Wearing a mask and practicing cough etiquette according to the situation
- Understanding and practicing lifestyle habits such as moderate exercise and diet
- Enforcement of ventilation, and avoiding crowded places, close contact, and closed spaces (the 3 Cs)
- Make efforts such as promoting the use of telework in the workplace.
- From May 8 this year, the government will not uniformly request the use of basic infection control measures, but will respect the independent choice of individuals and leave it to their judgment.
- Test-positive persons on home care should monitor their own physical condition by such means as checking their body temperature and taking thorough measures against infection when going out. They must also be asked to avoid contact with people who are at risk of aggravation, such as elderly people.
- To allow the minimum necessary outings, such as shopping for groceries, after 24 hours have passed since symptoms have subsided or when there are no symptoms, it is necessary to take voluntary actions to prevent infection, such as wearing a mask when going out, keeping contact with other people at the minimum period of time possible, and not using public transportation.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is also considered to have occurred via droplets adhering to mucosa, aerosol inhalation, contact infection, etc.
- [Severity, etc.]
It has been shown that infection with the Omicron variant may present a relatively lower risk of hospitalization or aggravation than with the Delta variant. To evaluate COVID-19, including the Omicron variant, it is not only necessary to assess the severity as a disease but also of the transmissibility and the impact on the medical care system and society as a whole.
Concerning the death toll since the outbreak at the end of 2021, it is reported that the novel coronavirus is not the direct cause of death in quite a number of cases compared to the epidemic in the summer of 2021; for example, when elderly people who had been living in a facility for elderly people since before the infection were infected and died, the death was due to worsening of the underlying disease. There were many cases of serious respiratory failure due to typical viral pneumonia caused by the novel coronavirus infection from the beginning of the novel coronavirus outbreak until the outbreak of the Delta variant. However, during the Omicron variant outbreak, it was reported that diseases other than pneumonia became the main causes of death, such as exacerbation of the underlying disease that had been present before hospitalization and the onset of other complications during hospitalization.
Concerning the spread of infection last summer, there has been a continuing decrease in the rate of severe cases and increase in the ratio of elderly people among hospitalized patients as during the previous outbreak compared to the spread of the infection in the summer of 2021. Compared to the spread of infection from the end of 2021, the number of deaths in the spread of infection last summer is lower than the rate of mechanical ventilation/nasal high flow use and the steroid prescription rate.
Among the fatal cases of infected children who died of endogenous factors, there were some cases without any underlying diseases. The reports on the results of on-site investigations have stated that it is necessary to pay attention to neurological symptoms such as convulsions and disturbance of consciousness, and systemic symptoms such as vomiting and poor oral intake besides the respiratory symptoms.
Among the deaths that occurred at home in July and August last year, approximately 80% of the patients were 70 years and older, which is similar to the trend of all deaths during the same period. It suggests that there were also many deaths caused by factors other than COVID-19. Regarding the situation of handling dead bodies known to be coronavirus positive, the number of cases reported monthly was the highest last December. The proportion of deaths due to COVID-19 has reached approximately 30% of all deaths.
- [Virus shedding period]
According to Japanese data, the risk of infection remains until 10 days after the onset, and infectivity is high until 7 days after the onset. Even after waiting for 5 days, a third of the patients are still shedding infectious viruses. On Day 8 (after isolation for 7 days), most patients (approximately 85%) did not shed infectious viruses, and it was reported that even if patients did shed the virus, the amount of virus decreased to one-sixth that in the initial stage of onset after 7 days.
- [Vaccine effects]
Concerning the conventional vaccine, the infection and disease onset prevention effects of the first vaccination against the Omicron variant are markedly reduced. The hospitalization-preventing effect is reported maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing, disease onset-preventing and hospitalization-preventing effects against infection with the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Concerning the vaccine against the Omicron variant (BA.4-5), it has been reported that the preventive effect against disease onset was observed within 0 to 2 months (median 1 month) after vaccination.
- [Sublineages of the Omicron Variant]
The proportion of the BA.5 lineage, which was the mainstream worldwide, is declining, and currently the proportion of the XBB lineage (the BJ.1 lineage [a sublineage of the BA.2.10 lineage]), including the XBB.1.5 lineage is seen to be increasing. Increases in the number and proportion have been observed in the United States in the XBB.1.5 lineage, which is a sublineage of the XBB lineage, and in Europe and the United States in the XBB.1.9 lineage (including sublineages in both). Although the severity of the XBB.1.5 lineage is not greater than that of the BQ.1 lineage, otherwise the clinical picture and epidemiological findings are insufficient. While the clinical picture and epidemiological findings on the XBB.1.9 lineage are not yet sufficient, it is necessary to continue collecting and analyzing data on overseas situations, and to continue monitoring by genome surveillance. However, since the number of registered mutant strains is decreasing as the number of infected people decreases worldwide, caution is required when considering the proportion of mutant strains.
Figures (Number of new infections reported etc.) (PDF)
- Details
119th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (March 23, 2023)Material 1
Evaluation of the latest infection status, etc.
Overview of the infection status, etc.
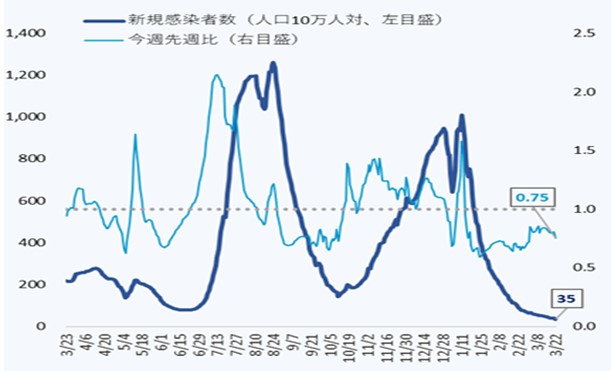
- The number of new cases of infection nationwide was approximately 35 per 100,000 of the population in the last week, showing a continuous decreasing trend with a ratio of this week to last week of 0.75.
It is necessary to pay attention to situations where the risk of infection increases at the change of the fiscal year, and the impact on the infection situation of the attenuation of immunity and replacement by variant strains. - The use rate of beds has been decreasing nationwide, and the numbers of severe cases and deaths have also continued to decrease.
Reference: Local trend
* The number of new cases of infection is an approximate figure per 100,000 of the population, as the total for the current week, which is the reported number in HER-SYS as of Mar. 22, 00:00 AM (the same time point is used for the ratio to the previous week), and the use rate of beds is the secured bed use rate as of the time of writing this document on Mar. 22.
Infection status and future outlook
Infection status
- The number of new cases of infection shows a continuous decreasing trend nationwide, and the ratio to the previous week remains below 1.0 in almost all prefectures. The level is below that before the spread of infection in the summer of last year, and the decrease in the number of new cases of infection has been decreasing.
- Regarding the number of new cases of infection by region, in the Hokuriku-Koshinetsu and Chugoku-Shikoku regions, the number per population is higher than the national average. Meanwhile, in the Kanto and Kinki regions, the number is lower than the average. In addition, there is a continuous decreasing trend in mass infections in facilities for elderly people, medical institutions, etc.
- The number of new cases of infection nationwide by age group shows a decreasing trend in all age groups, and the difference between age groups per 100,000 population is also decreasing.
- The numbers of severe cases and deaths continue to show a downward trend nationwide. With the spread of infection this winter, the proportion of elderly patients in their 80s and older among newly infected patients tended to increase, compared to that during the spread of infection in the summer last year.
- As the reports of deaths among children since January 2022 suggest, attention must be paid to the occurrence of severe cases and deaths as well as the number of hospitalized children associated with an increase in the number of infected children.
- The incidence of seasonal influenza is lower than usual during the same period nationwide, but higher than in the last two years. At the time of the announcement last weekend, the number of cases reported weekly per fixed-point medical institution increased slightly nationwide compared to the previous week, and the number remains above 10 and at the advisory level.
Future outlook
- Regarding the future infection status, it is expected that the number of new cases of infection will continue to be flat nationwide based on the epi curve and the short-term forecast nationwide and in large cities, although there are regional differences and uncertainty. In some regions, however, it may increase toward the end of March. It is necessary to pay attention to future situations where the risk of infection increases at the change of the fiscal year, and the impact on the infection situation of the attenuation of immunity and increase in the proportion of strains with the ability to escape the immune system.
- The incidence of seasonal influenza is expected to continue to decrease in the future based on past trends, but attention should be paid continuously.
Factors that increase and suppress infection
- [Immunity as a result of vaccination and infection]
With the promotion of vaccination and natural infection, the proportion of immune carriers against the Omicron variant (BA.5 and BQ1.1), which has shown an increase in each age group, is thought to decrease over time in the future.
- [Contact status]
The nighttime population is currently trending downward in many regions, but there are also regions where it is increasing. In addition, the number of opportunities for contact is expected to increase due to spring vacation and the new fiscal year.
- [Epidemic strains]
Currently, the BA.5 lineage is the mainstream in Japan, but sublineages of the Omicron variant such as BQ.1 and XBB lineages, particularly XBB.1.5, which has been reported mainly in the US, are considered to have an enhanced ability to escape the immune system, and have been pointed out to predominate among the increasing number of infected people overseas. The BQ.1 lineage, which was increasing in number and proportion in Japan, has been decreasing since peaking in early January. On the other hand, it is estimated that the proportions of the BQ.1 and XBB.1.5 lineages will increase in the future, and close attention is needed. The proportion of the BN.1.3 lineage, which is a sublineage of the BA.2.75 lineage, has also been increasing in Japan.
- [Climatic and seasonal factors]
Ventilation is difficult on days with low temperatures. Attention should also be paid to respiratory viral infections.
Situation of the medical care provision system
- The use rate of beds shows a decreasing trend nationwide and is at a low level below 20% in all regions. The use rate of beds for severe cases is also low nationwide.
- The number of patients receiving treatment in nursing care facilities has continued to decrease.
- Regarding emergency medical care, the number of cases of difficult emergency transport has been decreasing nationwide, but attention should continuously be paid to the future trend of the number of cases having difficulty with emergency transportation and securing a system to provide emergency medical care.
Measures to be taken
Basic concepts
- Unless we face special circumstances such as the emergence of a variant with a pathogenicity greatly different from that of the Omicron variant, COVID-19 shall be positioned as a Class V Infectious Disease instead of a Novel Influenza Infection, etc. under the Infectious Disease Act from May 8 this year (2023). In association with this, the government decided on March 10 this year to make necessary revisions to various policies and measures that have been taken, such as the medical care system, response to facilities for the elderly, and public financial support for patients.
- Meanwhile, it is necessary to continue efforts to strengthen and focus the healthcare system to provide appropriate medical care for elderly people and those at high risk of aggravation, even with limited medical resources.
- Each citizen will be asked to take voluntary actions to prevent infection to protect those at high risk of aggravation, such as elderly people, and to ensure regular medical care.
- 1. Further promotion of vaccination
- As for the “vaccine for the Omicron variant," vaccination of all persons aged 5 and older who have completed the first vaccination should proceed.
- As both vaccines for the BA.1 and the BA.4 and BA.5 lineages are expected to be more effective than the previous vaccines, it is necessary to proceed with vaccination with the vaccine that can be given sooner. All eligible persons who wish to receive vaccination will be asked to receive the vaccine for the Omicron variant.
- Those who have not received vaccination will be encouraged to consider getting the initial vaccination as soon as possible.
- For children (aged 5 to 11 years), the initial vaccination and additional vaccination with the vaccine for the Omicron variant will be promoted. For children (aged 6 months to 4 years), the initial vaccination will be promoted.
- Vaccination in FY 2023 will be promoted (vaccination will be given to all eligible persons aged 5 years and older in autumn and winter, and additional vaccination will be given to elderly people and those at high risk of aggravation as well as spring and summer).
- 2. Use of tests
- The national and local governments are required to secure a system that enables testing, and should utilize testing.
- Perform frequent tests (about 2 or 3 times a week for facility workers) for workers at facilities for elderly people.
- Promote the establishment of a system for fever outpatients, whereby patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Promote the utilization of antigen qualitative test kits, which have been switched to OTC and are sold on the Internet.
- 3. Securing a medical care provision system
- With support of the national government, local governments continue to take measures to avoid overcrowding of hospital beds, fever clinics, etc.
- Make appropriate adjustments so that patients who need hospital treatment can be hospitalized preferentially (securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule). Implement frequent examinations at facilities for elderly people and others. Further strengthen medical support during normal times.
- Local residents should be informed that they should refrain from visiting emergency outpatient units only to receive a precautionary examination if they do not have symptoms, for example, taking the actual situation in the region into consideration, so that nobody is prevented from receiving treatment. To respond to concerns and questions when a patient’s physical condition deteriorates, the telephone consultation service by healthcare professionals should be thoroughly publicized, and this service should also be strengthened.
- In response to the government's decision on March 10 this year, with the change in positioning as a Class V Infectious Disease, encourage medical facilities that have been responding to the new coronavirus infection to continue to respond, and start efforts to encourage new medical facilities to participate.
- Maintenance and expansion of responding medical institutions through review of infection control measures, support for maintenance of facilities, clarification of the obligation to provide treatment, and dissemination of easy-to-understand educational materials on infection control and medical treatment policies
- In each prefecture, until the expansion of infection in the next winter a transition plan up to the end of September will be formulated in April, with contents such as the acceptance of patients with mild disease by new medical institutions, and the coordination of hospitalization among medical institutions.
- 4. Response to simultaneous epidemics of COVID-19 and seasonal influenza
- The following efforts should be promoted according to the actual situation in each region: strengthening of the fever outpatient clinics, strengthening of telephone consultations/telemedicine, expansion of health follow-up centers, securing of self-test kits, strengthening of the consultation system, and prevention of overcrowded emergency medical care.
- Smooth supply of medications including oral drugs prescribed after confirmation of the indication by physicians will be promoted. Pharmacies, etc. will be asked to use the consultation service of the Ministry of Health, Labour and Welfare when it is difficult to obtain antipyretic analgesics.
- The prefectures will work to strengthen and prioritize the health care system based on plans to establish systems such as strengthening of outpatient medical care systems in accordance with the actual conditions in each region.
- It is necessary to provide information and send appropriate messages to the public depending on the infection status. People at low risk of aggravation will be encouraged to use a self-test kit or local follow-up center.
- People will be advised to do the following: check the “guide for ambulance services” in preparation for an acute illness or injury, consult a family doctor when hesitant to call an ambulance, use a telephone consultation service such as #7119, and call an ambulance without hesitation if necessary.
- 5. Surveillance and risk assessment, etc.
- It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status. It is also necessary to continue monitoring of the trends of variants through genomic surveillance.
- Regarding the risk assessment of COVID-19, it is necessary to continue evaluation of the pathogenicity, infectivity, mutations, etc.
- 6. Quarantine measures
- Temporary measures have been taken for entrants from China from December 30 last year. The positive rate among entrants has been at a relatively low level, and all of the variants observed so far are lineages of the Omicron variant with a history of detection in Japan. Taking these accumulated findings and other circumstances into consideration, screening at the time of entry was changed from testing of all entrants to sample testing of some entrants from March 1. Flexible responses will be given while observing the infection status in China, etc.
- 7. Effective ventilation
- It is necessary to publicize and recommend effective ventilation methods to prevent insufficient indoor ventilation (such as how to create airflow considering aerosols, installation of partitions that do not block airflow).
- 8. Re-inspection and implementation of basic infection control measures
Everyone must take the following basic precautions from the perspective of being aware of the epidemic of infectious disease in the community, protecting ourselves from infectious disease, and protecting people close to us as well as society from infectious disease, especially the elderly.
- If feeling unwell or having symptoms, do not overdo it, and be treated at home or see a doctor.
- Hand hygiene such as hand washing as a daily habit
- Wearing a mask and practicing cough etiquette according to the situation
- Understanding and practicing lifestyle habits such as moderate exercise and diet
- Enforcement of ventilation, and avoiding crowded places, close contact, and closed spaces (the 3 Cs)
- Make efforts such as promoting the use of telework in the workplace.
- From March 13 this year, the government will not uniformly request mask-wearing as a rule, but will respect the independent choice of individuals and leave the use of masks to their judgment.
- Test-positive persons on home care should monitor their own physical condition by such means as checking their body temperature and taking thorough measures against infection when going out. They must also be asked to avoid contact with people who are at risk of aggravation, such as elderly people.
- To allow the minimum necessary outings, such as shopping for groceries, after 24 hours have passed since symptoms have subsided or when there are no symptoms, it is necessary to take voluntary actions to prevent infection, such as wearing a mask when going out, keeping contact with other people at the minimum period of time possible, and not using public transportation.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is also considered to have occurred via droplets adhering to mucosa, aerosol inhalation, contact infection, etc.
- [Severity, etc.]
It has been shown that infection with the Omicron variant may present a relatively lower risk of hospitalization or aggravation than with the Delta variant. To evaluate COVID-19, including the Omicron variant, it is not only necessary to assess the severity as a disease but also of the transmissibility and the impact on the medical care system and society as a whole.
Concerning the death toll since the outbreak at the end of 2021, it is reported that the novel coronavirus is not the direct cause of death in quite a number of cases compared to the epidemic in the summer of 2021; for example,when elderly people who had been living in a facility for elderly people since before the infection were infected and died, the death was due to worsening of the underlying disease. There were many cases of serious respiratory failure due to typical viral pneumonia caused by the novel coronavirus infection from the beginning of the novel coronavirus outbreak until the outbreak of the Delta variant. However, during the Omicron variant outbreak, it was reported that diseases other than pneumonia became the main causes of death, such as exacerbation of the underlying disease that had been present before hospitalization and the onset of other complications during hospitalization.
Concerning the spread of infection last summer, there has been a continuing decrease in the rate of severe cases and increase in the ratio of elderly people among hospitalized patients as during the previous outbreak compared to the spread of the infection in the summer of 2021. Compared to the spread of infection from the end of 2021, the number of deaths in the spread of infection last summer is lower than the rate of mechanical ventilation/nasal high flow use and the steroid prescription rate.
Among the fatal cases of infected children who died of endogenous factors, there were some cases without any underlying diseases. The reports on the results of on-site investigations have stated that it is necessary to pay attention to neurological symptoms such as convulsions and disturbance of consciousness, and systemic symptoms such as vomiting and poor oral intake besides the respiratory symptoms.
Among the deaths that occurred at home in July and August last year, approximately 80% of the patients were 70 years and older, which is similar to the trend of all deaths during the same period. It suggests that there were also many deaths caused by factors other than COVID-19. Regarding the situation of handling dead bodies known to be coronavirus positive, the number of cases reported monthly has been the highest during last December. The proportion of deaths due to COVID-19 has reached approximately 30% of all deaths.
- [Virus shedding period]
According to Japanese data, the risk of infection remains until 10 days after the onset, and infectivity is high until 7 days after the onset. Even after waiting for 5 days, a third of the patients are still shedding infectious viruses. On Day 8 (after isolation for 7 days), most patients (approximately 85%) did not shed infectious viruses, and it was reported that even if patients did shed the virus, the amount of virus decreased to one-sixth that in the initial stage of onset after 7 days.
- [Vaccine effects]
Concerning the conventional vaccine, the infection and disease onset prevention effects of the first vaccination against the Omicron variant are markedly reduced. The hospitalization-preventing effect is reported maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing, disease onset-preventing and hospitalization-preventing effects against infection with the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Concerning the vaccine against the Omicron variant (BA.4-5), it has been reported that the preventive effect against disease onset was observed within 0 to 2 months (median 1 month) after vaccination.
- [Sublineages of the Omicron variant]
While the BA.5 lineage continues to be mainstream in the world, its proportion has been decreasing slightly, and other sublineages and recombinants of the Omicron variant with characteristic mutations in the spike protein have been reported worldwide. In particular, the proportions of the XBB lineage (a recombinant of the BJ.1 lineage (a sublineage of the BA.2.10 lineage) and the BM.1.1.1 lineage (a sublineage of the BA.2.75.3 lineage)) and the XBF lineage (a recombinant of the BA.5.2.3 lineage and the CJ.1 lineage (a sublineage of BA.2.75.3 lineage)) have increased relatively. The numbers and proportions of the XBB.1.5 lineage, which is a sublineage of the XBB lineage, have increased in the United States, as have the XBF lineage in Australia, and the XBB.1.9 strain (including sublineages) in Europe and the United States. Although the clinical picture and epidemiological findings on the XBB.1.9 lineage are not yet sufficient, it is necessary to continue collecting and analyzing data on overseas situations and findings regarding the characteristics of these new sublineages and recombinants, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)
- Details
Updated March 24, 2023, at 9:00 am
National Institute of Infectious Diseases, Japan
*This is a provisional translation of the summary of the report entitled "kansen-denpasei no zoukaya kougenseino henkaga kenensareru SARS-CoV-2 no henikabunituite (dai26hou) (https://www.niid.go.jp/niid/ja/2019-ncov/2551-cepr/11879-sars-cov-2-26.html)". In the case of any dispute over translation, Japanese text prevails.
Overview of SARS-CoV-2 variants
The Omicron, the B.1.1.529, and its descendent lineages are still dominant globally among SARS-CoV-2 variants, with no significant changes in epidemiological trends compared to the No. 25 report. The World Health Organization (WHO) refers to all B.1.1.529 sub-lineages and recombinants as Omicron, whereas NIID has classified omicron variants as variants of concern (VOCs).
The omicron variants are genetically divergent, and WHO and European Centre for Disease Prevention and Control (ECDC) have classified them as variants under monitoring (VUM), variants of interest (VOIs), and VOCs. The WHO has classified XBB.1.5 as currently circulating variants of interest (VOIs), and BQ.1, BA.2.75, CH.1.1, XBB and XBF as currently circulating variants under monitoring (VUMs), respectively, since March 15. However, the information lacks significant changes in viral characteristics such as severity or infectivity/transmissibility, apart from the predominance of the increased number of infected cases and the possibility of immune escape between subvariants. Thus, NIID continues the current classification of the subvariants. It is important to continue monitoring and collecting information on sub-variant outbreaks through genomic analysis in the country and quarantine.
They accounted for 98.4% of the sequences submitted to GISAID from February 13 to March 13, with few reports of other lineages (WHO, 2023). The XBB variant accounted for 44.8% of the detected subvariants and became dominant in five of the six WHO regions, except the Western Pacific region, in the 8th week of 2023 (February 20-26).
The top three variants globally were XBB.1.5 (35.1%), BQ.1 (15.1%), and XBB, excluding XBB.1.5 (9.7) (WHO, 2023). In Japan, BA.5 replaced BA.2 around July 2022, and the relative sequence prevalence among circulating variants has been dominated by BA.5, followed by an increasing proportion of BQ.1 (a sub-lineage of the BA.5.3 lineage) and BA.2.75 (a sub-lineage of the BA.2 lineage) since October 2022.
Some subvariants, such as BQ.1 and XBB, exhibit characteristic mutations in the spike protein that allow the virus to evade neutralizing antibodies through vaccination, infection, and/or show a growth advantage. Some subvariants, such as XBB.1.5, are increasing in North America and may have a growth advantage over existing sub-lineages in certain regions. However, there were no findings that they spread more rapidly than the other variants.
Omicron subvariants have emerged with specific characteristics that primarily contribute to immune escape. There were no significant differences from the other variants except for them. Global immune status and some public health interventions in each country have resulted in less influence of variant-specific nature on epidemic dynamics. It is crucial to determine appropriate interventions based on regular monitoring of variant prevalence and changes in variant-specific features, including virulence, transmissibility, vaccine and antiviral resistance, clinical presentation, and rapid risk assessment for each variant.
COVID-19 surge has been reported in China since November 2022. China decided to cease the zero-COVID-19 policy on December 7, 2022. The number of daily cases started increasing in late December 2022, and there was a late increase in severe or hospitalized patients in early January 2023. Recent reports have demonstrated a decreasing trend in the number of daily cases. According to sequences submitted to GISAID from China, BA.5.2.48 and BF.7.14 were considered dominant. These subvariants are thought to have no significant effect on immune escape, transmissibility, and severity compared with BA.5.2 and BF.7, which have already been detected in Japan.
Japan conducted screening tests for all passengers with a travel history of China (excluding Hong Kong and Macau) (within seven days) and all passengers directly from China (excluding Hong Kong and Macau) as they arrived from December 30, 2022. These test results revealed that BA.5.2 and BF.7 are dominant in these passengers from China. The quarantine testing policy has changed since March 1 to test a maximum of 20% of the samples from passengers from China (excluding Hong Kong and Macau).
- Details
118th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (March 8, 2023) Material 1
Evaluation of the latest infection status, etc.
Overview of the infection status, etc.
- The number of new cases of infection nationwide was approximately 57 per 100,000 of the population in the last week, showing a continuous decreasing trend with a ratio of this week to last week of 0.81.
It is necessary to pay attention to the future impacts of attenuation of immunity and replacement by variant strains on the infection status. - The use rate of beds has been decreasing nationwide, and the numbers of severe patients and deaths have also continued to decrease.
Reference: Local trend
*The number of new cases of infection is an approximate figure per 100,000 of the population, as the total for the current week, which is the reported number in HER-SYS as of Mar. 7, 00:00 AM (the same time point is used for the ratio to the previous week), and the use rate of beds is the secured bed use rate as of the time of writing this document on Mar. 7.
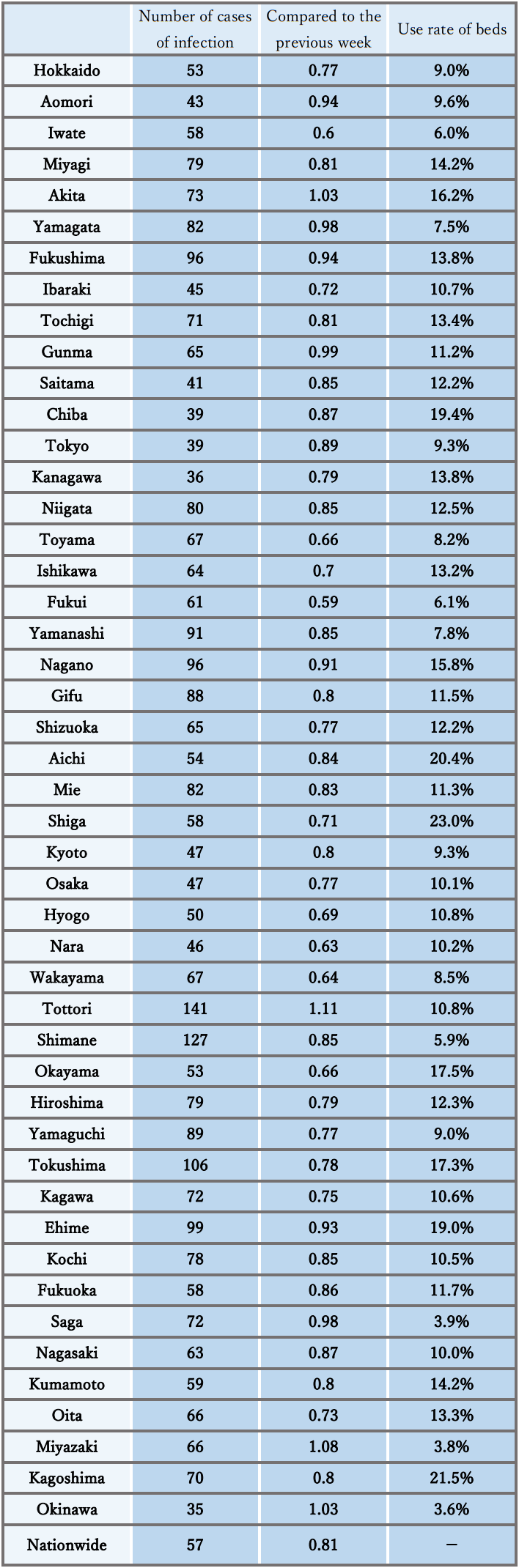
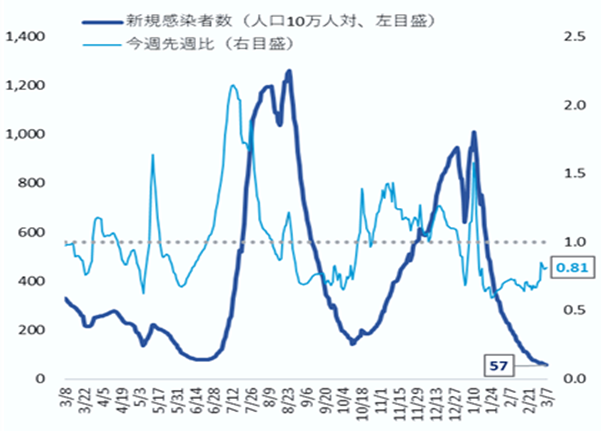
Infection status and future outlook
Infection status
- The number of new cases of infection shows a continuous decreasing trend nationwide, and the ratio to the previous week remains below 1.0 in most prefectures. The level is below that before the spread of infection in the summer of last year, and the decrease in the number of new cases of infection has been decreasing.
- Regarding the number of new cases of infection by region, in the Chugoku and Shikoku regions, the number per population is higher than the national average. Meanwhile, in the Kanto region and Okinawa, the number is lower than the average. In addition, there is a continuous decreasing trend in mass infections in facilities for elderly people, medical institutions, etc.
- The number of new cases of infection nationwide by age group shows a decreasing trend in all age groups, and the difference between age groups is smaller.
- The numbers of severe cases and deaths continue to show a downward trend nationwide. With the spread of infection this winter, the proportion of elderly patients in their 80s and older among newly infected patients tended to increase, compared to that during the spread of infection in the summer last year.
- As the reports of deaths among children since January 2022 suggest, attention must be paid to the occurrence of severe cases and deaths as well as the number of hospitalized children associated with an increase in the number of infected children.
- The incidence of seasonal influenza is lower than that during the same period of usual years, but higher than that during the same period of the last 2 years. At the time of announcement last weekend, the number of cases reported weekly per fixed-point medical institution had slightly decreased nationwide, compared to the previous week. But it is still at advisory level exceeding 10 nationwide, and at alert level exceeding 30 in Ishikawa, Iwate, and Fukui.
Future outlook
- Regarding the future infection status, it is expected that the number of new cases of infection will continue to be flat nationwide based on the epi curve and the short-term forecast nationwide and in large cities, although there are regional differences and uncertainty. In some regions, however, it may increase toward the end of March. It is necessary to pay attention to whether or not the increasing trend in regions with a ratio to the previous week of more than 1 will continue in the future, as well as the future impact of attenuation of immunity, an increase in the proportion of strains with potential to escape the immune system, and other factors on the infection status.
- The incidence of seasonal influenza is expected to continue to show a decreasing trend based on past trends, but attention should be paid continuously.
Factors that increase and suppress infection
- [Immunity as a result of vaccination and infection]
With the promotion of vaccination and natural infection, the proportion of immune carriers against the Omicron variant (BA.5 and BQ1.1) shows an increase in each age group, and it has been reported that the percentage is increasing particularly in the elderly population because of vaccination. However, immunity acquired from vaccination and natural infection may decline over time.
- [Contact status]
The nighttime population has been flat overall, although it has lately increased or decreased in some regions.
- [Epidemic strains]
Currently, the BA.5 lineage is the mainstream in Japan, but sublineages of the Omicron variant such as BQ.1 and XBB lineages, particularly XBB.1.5, which has been reported mainly in the US, are considered to have an enhanced ability to escape the immune system, and have been pointed out to predominate among the increasing number of infected people overseas. In Japan, the proportion of the BQ.1 lineage showed an increasing trend before but has been decreasing for 3 consecutive weeks. On the other hand, the proportion of the XBB.1.5 lineage seems to be increasing, and therefore attention needs to be paid. The proportion of the BN.1.3 lineage, which is a sublineage of the BA.2.75 lineage, has also been increasing in Japan.
- [Climatic and seasonal factors]
Days with low temperatures nationwide make ventilation difficult. Attention should also be paid to respiratory viral infections.
Situation of the medical care provision system
- The use rate of beds shows a decreasing trend nationwide and is at a low level below 30% in all regions. The use rate of beds for severe cases is also low nationwide.
- The number of patients receiving treatment in nursing care facilities has continued to decrease.
- In emergency medical care, the number of cases having difficulty with emergency transportation had been decreasing nationwide before but has been flat recently. Attention should continuously be paid to the future trend of the number of cases having difficulty with emergency transportation and securing a system to provide emergency medical care.
Measures to be taken
Basic concepts
- Unless we face special circumstances such as the emergence of a variant with a pathogenicity greatly different from that of the Omicron variant, COVID-19 shall be positioned as a Class V Infectious Disease instead of a Novel Influenza Infection, etc. under the Infectious Disease Act from May 8 this year (2023). In association with this, various policies and measures taken will be reviewed.
- Meanwhile, it is necessary to continue efforts to strengthen and focus the healthcare system to provide appropriate medical care for elderly people and those at high risk of aggravation, even with limited medical resources.
Each citizen will be asked to take voluntary actions to prevent infection to protect those at high risk of aggravation, such as elderly people, and to ensure regular medical care.
- 1. Further promotion of vaccination
- As for the “vaccine for the Omicron variant," vaccination of all persons aged 5 and older who have completed the first vaccination should proceed.
- As both vaccines for the BA.1 lineage and the BA.4 and BA.5 lineages are expected to be more effective than the previous vaccines, it is necessary to proceed with vaccination with either vaccine, whichever can be given sooner.
All eligible persons who wish to receive vaccination will be asked to receive the vaccine for the Omicron variant. - Those who have not received vaccination will be encouraged to consider getting the initial vaccination as soon as possible.
- For children (aged 5 to 11 years), the initial vaccination and additional vaccination with the vaccine for the Omicron variant will be promoted. For children (aged 6 months to 4 years), the initial vaccination will be promoted.
- Vaccination in FY 2023 will also be promoted (vaccination will be given to all eligible persons aged 5 years and older in autumn and winter, and additional vaccination will be given to elderly people and those at high risk of aggravation as well as spring and summer).
- 2. Use of tests
- The national and local governments are required to secure a system that enables testing, and should utilize testing.
- Perform frequent tests (about 2 or 3 times a week for facility workers) for workers at facilities for elderly people.
- Promote the establishment of a system for fever outpatients, whereby patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Promote the utilization of antigen qualitative test kits, which have been switched to OTC and are sold on the Internet.
- 3. Quarantine measures
- Temporary measures have been taken for entrants from China from December 30 last year. The positive rate among entrants has been at a relatively low level, and all of the variants observed so far are lineages of the Omicron variant with a history of detection in Japan. Taking these accumulated findings and other circumstances into consideration, screening at the time of entry has been changed from testing of all entrants to sample testing of some entrants from March 1. Flexible responses will be given while observing the infection status in China, etc.
- 4. Securing a medical care provision system
With support of the national government, local governments are required to take measures to avoid overcrowding of hospital beds, fever clinics, etc.
- Maintain the total number of beds required for patients infected with COVID-19 based on the bed securing plan. In addition, continue to increase the number of medical institutions that can handle COVID-19 by supporting improvement of the ability to treat COVID-19 cases, even at hospitals without any beds for infected patients (promotion of zoning of hospital rooms, etc.).
- Take immediate responses such as securing beds, and make efforts to avoid being overwhelmed concerning the number of hospital beds and emergency medical care by using lodging facilities and resting beds, for example.
- Make appropriate adjustments so that patients who need hospital treatment can be hospitalized preferentially (securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule). Implement frequent examinations at facilities for elderly people and others. Further strengthen medical support during normal times.
- In addition to extending the office hours and the number of outpatient clinics for fever patients, the outpatient medical care system is strengthened and prioritized by strengthening regional outpatient and testing centers and telephone and online clinics, etc.
- Local residents should be informed that they should refrain from visiting emergency outpatient units only to receive a precautionary examination if they do not have symptoms, for example, taking the actual situation in the region into consideration, so that nobody is prevented from receiving treatment. To respond to concerns and questions when a patient’s physical condition deteriorates, telephone consultation services by healthcare professionals should be thoroughly publicized, and this service should also be strengthened.
- 5. Response to simultaneous epidemics of COVID-19 and seasonal influenza
- The following efforts should be promoted according to the actual situation in each region: strengthening of the fever outpatient clinics, strengthening of telephone consultations/telemedicine, expansion of health follow-up centers, securing of self-test kits, strengthening of the consultation system, and prevention of overcrowded emergency medical care.
Smooth supply of medications including oral drugs prescribed after confirmation of the indication by physicians will be promoted. Pharmacies, etc. will be asked to use the consultation service of the Ministry of Health, Labour and Welfare when it is difficult to obtain antipyretic analgesics. - The prefectures will work to strengthen and prioritize the health care system based on plans to establish systems such as strengthening of outpatient medical care systems in accordance with the actual conditions in each region.
- It is necessary to provide information and send appropriate messages to the public depending on the infection status. People at low risk of aggravation will be encouraged to use a self-test kit or local follow-up center.
- People will be advised to do the following: check the “guide for ambulance services” in preparation for an acute illness or injury, consult a family doctor when hesitant to call an ambulance, use a telephone consultation service such as #7119, and call an ambulance without hesitation if necessary.
- At the same time, vaccination against COVID-19 and seasonal influenza of those who are subject to vaccination should be promoted.
- The following efforts should be promoted according to the actual situation in each region: strengthening of the fever outpatient clinics, strengthening of telephone consultations/telemedicine, expansion of health follow-up centers, securing of self-test kits, strengthening of the consultation system, and prevention of overcrowded emergency medical care.
- 6. Surveillance and risk assessment, etc.
- It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status. It is also necessary to continue monitoring of the trends of variants through genomic surveillance.
- Regarding the risk assessment of COVID-19, it is necessary to continue evaluation of the pathogenicity, infectivity, mutations, etc.
- 7. Effective ventilation
- It is necessary to publicize and recommend effective ventilation methods to prevent insufficient indoor ventilation (how to create airflow considering aerosols and installation of partitions that do not block the airflow, for example) due to the use of heating appliances on days with low temperatures.
- 8. Re-inspection and implementation of basic infection control measures
Re-inspection and implementation of the following basic infection control measures are needed.
- Continue proper wearing of nonwoven masks according to the situation, hand hygiene, thorough ventilation, etc.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, or loud voices.
- In the event of a meeting at a restaurant, choose a venue certified by a third party, keep the number of people as low as possible, avoid speaking in loud voices and staying for a long time, and wear a mask when talking.
- People with symptoms such as sore throat, cough, and fever should refrain from going out.
- Refer to guidelines for hospital visits and use of an ambulance.
- Prepare antigen qualitative test kits and antipyretic analgesics at home, and check the contact information of consultation services.
- Make efforts such as promoting the use of telework in the workplace.
- The organizers of events or meetings should examine and evaluate the epidemic status in the concerned region as well as the risk of infection, and then take measures to reduce the risk.
- From March 13 this year, the government will not uniformly request mask-wearing as a rule, but will respect the independent choice of individuals and leave the use of masks to their judgment. Until then, actions will be taken according to the previous policy.
- Test-positive persons on home care should monitor their own physical condition by such means as checking their body temperature and taking thorough measures against infection when going out. They must also be asked to avoid contact with people who are at risk of aggravation, such as elderly people.
- To allow the minimum necessary outings, such as shopping for groceries, after 24 hours have passed since symptoms have subsided or when there are no symptoms, it is necessary to take voluntary actions to prevent infection, such as wearing a mask when going out, keeping contact with other people at the minimum period of time possible, and not using public transportation.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is also considered to have occurred via droplets adhering to mucosa, aerosol inhalation, contact infection, etc.
- [Severity, etc.]
It has been shown that infection with the Omicron variant may present a relatively lower risk of hospitalization or aggravation than with the Delta variant. To evaluate COVID-19, including the Omicron variant, it is not only necessary to assess the severity as a disease but also of the transmissibility and the impact on the medical care system and society as a whole.
Concerning the death toll since the outbreak at the end of 2021, it is reported that the novel coronavirus is not the direct cause of death in quite a number of cases compared to the epidemic in the summer of 2021; for example, when elderly people who had been living in a facility for elderly people since before the infection were infected and died, the death was due to worsening of the underlying disease. There were many cases of serious respiratory failure due to typical viral pneumonia caused by the novel coronavirus infection from the beginning of the novel coronavirus outbreak until the outbreak of the Delta variant. However, during the Omicron variant outbreak, it was reported that other diseases than pneumonia became the main causes of death, such as exacerbation of the underlying disease that had been present before hospitalization and the onset of other complications during hospitalization.
Concerning the spread of infection last summer, there has been a continuing decrease in the rate of severe cases and increase in the ratio of elderly people among hospitalized patients as during the previous outbreak compared to spreading of the infection in the summer of 2021. Among the deaths during the 2022 summer outbreak, mechanical ventilation/nasal high flow use rates and steroid prescription rates were decreased compared to the end of 2021 outbreak.
Among the fatal cases of infected children who died of endogenous factors, there were some cases without any underlying diseases. The reports on the results of on-site investigations have stated that it is necessary to pay attention to neurological symptoms such as convulsions and disturbance of consciousness, and systemic symptoms such as vomiting and poor oral intake besides the respiratory symptoms.
Among the deaths that occurred at home in July and August last year, approximately 80% of the patients were 70 years and older, which is similar to the trend of all deaths during the same period. It suggests that there were also many deaths caused by factors other than COVID-19. Regarding the situation of handling dead bodies known to be coronavirus positive, the number of cases reported monthly has been the highest during last December. The proportion of deaths due to COVID-19 has recently reached approximately 30% of all deaths.
- [Virus shedding period]
According to Japanese data, the risk of infection remains until 10 days after the onset, and infectivity is high until 7 days after the onset. Even after waiting for 5 days, a third of the patients are still shedding infectious viruses. On Day 8 (after isolation for 7 days), most patients (approximately 85%) did not shed infectious viruses, and it was reported that even if patients did shed the virus, the amount of virus decreased to one-sixth that in the initial stage of onset after 7 days.
- [Vaccine effects]
Concerning the conventional vaccine, the infection and disease onset prevention effects of the first vaccination against the Omicron variant are markedly reduced. The hospitalization-preventing effect is reported maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing, disease onset-preventing and hospitalization-preventing effects against infection with the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Concerning the vaccine against the Omicron variant (BA.4-5), it has been reported that the preventive effect against disease onset was observed within 0 to 2 months (median 1 month) after vaccination.
- [Sublineages of the Omicron variant]
While the BA.5 lineage continues to be mainstream in the world, its proportion has been decreasing slightly, and other sublineages and recombinants of the Omicron variant with characteristic mutations in the spike protein have been reported worldwide. In particular, the proportions of the XBB lineage (a recombinant of the BJ.1 lineage (a sublineage of the BA.2.10 lineage) and the BM.1.1.1 lineage (a sublineage of the BA.2.75.3 lineage)) and the XBF lineage (a recombinant of the BA.5.2.3 lineage and the CJ.1 lineage (a sublineage of BA.2.75.3 lineage)) has increased relatively. An increase in proportion has been observed for the XBB.1.5 lineage (a sublineage of XBB lineage) in the US and for the XBF lineage in Australia and other countries. According to the World Health Organization (WHO), etc., it has been pointed out that a predominance of the XBB.1.5 lineage among the increasing number of infected people may be attributed to its ability to escape the immune system, but no findings demonstrating an increased severity in patients infected with the XBB.1.5 lineage has been obtained so far. There are also no clear findings on the BN.1.3 lineage, which has been increasing in Japan. It is necessary to continue collecting and analyzing data on overseas situations and findings regarding the characteristics of these new sublineages and recombinants, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)
- Details
117th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (February 22, 2023) Material 1
Evaluation of the latest infection status, etc.
Overview of the infection status, etc.
- The number of new cases of infection nationwide was approximately 100 per 100,000 of the population in the last week, showing a continuous decreasing trend with a ratio of this week to last week of 0.68.
It is necessary to pay attention to the future impact of attenuation of immunity and replacement by variant strains on the infection status. - The use rate of beds has been decreasing nationwide, and the number of deaths and emergency cases that are difficult to transport have also continued to decrease.
Reference: Local trend
* The number of new cases of infection is an approximate figure per 100,000 of the population, as the total for the current week, which is the reported number in HER-SYS as of Feb 21, 00:00 AM (the same time point is used for the ratio to the previous week), and the use rate of beds is the secured bed use rate as of the writing of this document on Feb 21.
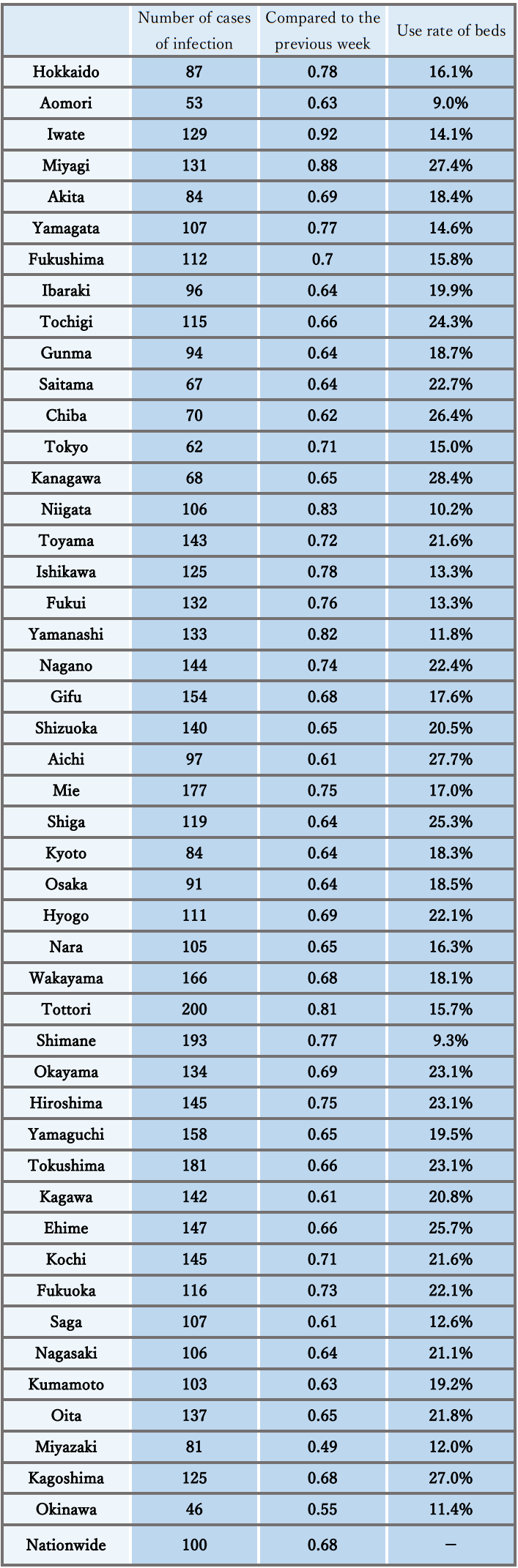
< Changes in the number of new cases of infection and comparison to the previous week (nationwide) >
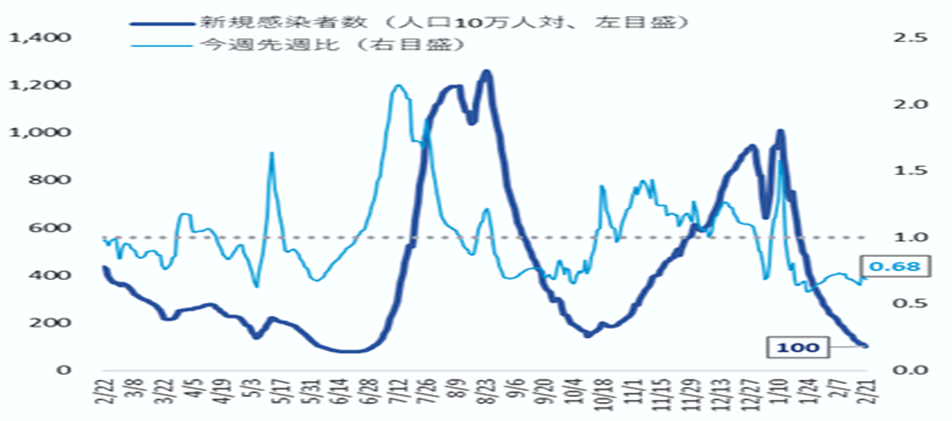
Infection status and future outlook
Infection status
- The number of new cases of infection shows a continuous decreasing trend nationwide, and the ratio to the previous week remains below 1.0 in all prefectures. It is also below the level before the spread of infection last autumn.
- Regarding the number of new cases of infection by region, in the Chugoku and Shikoku regions, the number per population is higher than the national average. Meanwhile, in the Kanto region and Okinawa, the number is lower than the average. However, the regional differences are also decreasing as the infection status improves. In addition, there is a decreasing trend in mass infections in facilities for elderly people, medical institutions, etc.
- The number of new cases of infection nationwide by age group shows a decreasing trend in all age groups, and also decreased even in the group of those under 10 years old that accounts for a large proportion of new cases of infection.
- The numbers of severe cases and deaths continue to show a downward trend nationwide. With the expansion of infection this winter, the proportion of elderly patients in their 80s and older among newly infected patients shows an increasing trend compared to that at the time of expansion of the infection the last summer. Attention should continuously be paid because the underlying diseases tend to deteriorate in winter.
- As the reports of deaths among children since January 2022 suggest, attention must be paid to the occurrence of severe cases and deaths as well as the number of hospitalized children associated with an increase in the number of infected children.
- The incidence of seasonal influenza is lower than during the same period in usual years, but higher than during the same period in the previous two years. At the time of the announcement last weekend, the number of cases reported weekly per fixed-point medical institution continued to exceed 10 nationwide, and the number exceeded 30 in Fukui, Ishikawa, and Okinawa. Both numbers have reached a warning level. Although the increasing trend continues nationwide, the rate of increase is smaller than the previous week.
Future outlook
- Regarding the future infection status, it is expected to show a continuous decreasing trend nationwide, despite regional differences and uncertainty, based on the epi curves and short-term forecasts nationwide and in large cities. It is necessary to pay attention to the future impact of the attenuation of immunity and an increase in the proportion of strains with the ability to escape the immune system on the infection status.
- Concerning the level of seasonal influenza, the increase in infection cases is expected to continue to decline based on past trends, and attention must still be paid to simultaneous infection of influenza and COVID-19.
Factors that increase and suppress infection
- [Immunity as a result of vaccination and infection]
With the promotion of vaccination and natural infection, the proportion of immune carriers against the Omicron variant (BA.5 and BQ1.1) shows an increase in each age group, and it has been reported that the percentage is increasing particularly in the elderly population because of vaccination. However, immunity acquired from vaccination and natural infection may decline over time.
- [Contact situation]
The nighttime population has recently increased in many areas but has decreased in some regions, showing regional differences.
- [Epidemic strains]
Currently, the BA.5 lineage is the mainstream in Japan, but sublineages of the Omicron variant such as BQ.1 and XBB lineages, particularly XBB.1.5, which has been reported mainly in the US, are considered to have an enhanced ability to escape the immune system, and have been pointed out to predominate among the increasing number of infected people overseas. Particularly regarding the BQ.1 lineage, the proportion is increasing domestically, and close attention is required. The proportion of BN.1.2 and BN.1.3 lineages, which are sublineages of the BA.2.75 lineage, has also increased in Japan.
- [Climatic and seasonal factors]
With the winter season, temperatures are dropping nationwide, making ventilation difficult. Respiratory virus infections also tend to be prevalent in winter.
Situation of the medical care provision system
- Nationwide, the use rate of beds generally shows a decreasing trend, and the rates in all areas are at a low level below 30%. The use rate of beds for severe cases is also low nationwide.
- The number of patients receiving treatment in nursing care facilities has been decreasing.
- As for emergency medical care, while the medical care system is usually overloaded in winter, the number of cases having difficulty with emergency transportation remains at a high level, but shows a continuous decreasing trend. Attention should continuously be paid to the future trend of the number of cases having difficulty with emergency transportation and securing a system to provide emergency medical care.
Measures to be taken
Basic concepts
- Unless we face special circumstances such as the emergence of a variant with a pathogenicity greatly different from that of the Omicron variant, COVID-19 shall be positioned as a Class V Infectious Disease instead of a Novel Influenza Infection, etc. under the Infectious Disease Act from May 8 this year (2023). In association with this, various policies and measures taken will be reviewed.
- Meanwhile, it is necessary to continue efforts to strengthen and focus the healthcare system to provide appropriate medical care for elderly people and those at high risk of aggravation, even with limited medical resources.
- Each citizen will be asked to take voluntary actions to prevent infection to protect those at high risk of aggravation, such as elderly people, and to ensure regular medical care.
- 1. Further promotion of vaccination
- As for the “vaccine for the Omicron variant," vaccination of all persons aged 12 and over who have completed the first vaccination should proceed.
- As both vaccines for the BA.1 and the BA.4 and BA.5 lineages are expected to be more effective than the previous vaccines, it is necessary to proceed with vaccination with the vaccine that can be given sooner. All eligible persons who wish to receive vaccination will be asked to receive the vaccine for the Omicron variant.
- Those who have not been vaccinated will be encouraged to consider getting the initial vaccination as soon as possible.
- Concerning children (ages 5 to 11), booster vaccinations will be promoted along with the initial vaccination. Concerning children (ages 6 months to 4 years), the initial vaccination will be promoted.
- It is necessary to promptly investigate how to use the novel coronavirus vaccine in the future.
- 2. Use of tests
- The national and local governments are required to secure a system that enables testing, and should utilize testing.
- Perform frequent tests (approximately 2 or 3 times a week) of facility workers at facilities for elderly people.
- Promote the establishment of a system for fever outpatients, whereby patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Promote the utilization of antigen qualitative test kits, which have been switched to OTC and are sold on the Internet.
- 3. Quarantine measures
- The COVID-19 situation in China is rapidly worsening, and it is difficult to grasp the details. Based on this situation, temporary measures such as immigration inspections have been implemented since December 30, 2022 to avoid a sharp increase in the inflow of COVID-19 into Japan, and flexible responses will be taken while monitoring the infection situation in China.
- 4. Securing a medical care provision system
In winter, it is also the time when the number of patients with diseases other than COVID-19 increase. With the support of the national government, prefectural governments must take measures to avoid overcrowding of hospital beds and fever outpatient clinics.
- Maintain the total number of beds required for patients infected with COVID-19 based on the bed securing plan. In addition, continue to increase the number of medical institutions that can handle COVID-19 by supporting improvement of the ability to treat COVID-19 cases, even at hospitals without any beds for infected patients (promotion of zoning of hospital rooms, etc.).
- Take immediate responses such as securing beds, and make efforts to avoid being overwhelmed concerning the number of hospital beds and emergency medical care by using lodging facilities and resting beds, for example.
- Make appropriate adjustments so that patients who need hospital treatment can be hospitalized preferentially (securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule). Implement frequent examinations at facilities for elderly people and others. Further strengthen medical support during normal times.
- In addition to extending the office hours and the number of outpatient clinics for fever patients, the outpatient medical care system is strengthened and prioritized by strengthening regional outpatient and testing centers and telephone and online clinics, etc.
- Local residents should be informed that they should refrain from visiting emergency outpatient units only to receive a precautionary examination if they do not have symptoms, for example, taking the actual situation in the region into consideration so that nobody is prevented from receiving treatment. To respond to concerns and questions when a patient’s physical condition deteriorates, the telephone consultation service by healthcare professionals should be thoroughly publicized, and this service should also be strengthened.
- Ensuring that test certificates are not required at workplaces and schools to start medical treatment.
- 5. Response to simultaneous epidemics of COVID-19 and seasonal influenza
- The following efforts should be promoted according to the actual situation in each region: strengthening of the fever outpatient clinics, strengthening of telephone consultations/telemedicine, expansion of health follow-up centers, securing of self-test kits, strengthening of the consultation system, and prevention of overcrowded emergency medical care.
- Smooth supply of medications including oral drugs prescribed after confirmation of the indication by physicians will be promoted. Pharmacies, etc. will be asked to use the consultation service of the Ministry of Health, Labour and Welfare when it is difficult to obtain antipyretic analgesics.
- The prefectures will work to strengthen and prioritize the health care system based on plans to establish systems such as strengthening of outpatient medical care systems in accordance with the actual conditions in each region.
- It is necessary to provide information and send appropriate messages to the public depending on the infection status. People at low risk of aggravation will be encouraged to use a self-test kit or local follow-up center.
- People will be advised to do the following: check the “guide for ambulance services” in preparation for an acute illness or injury, consult a family doctor when hesitant to call an ambulance, use a telephone consultation service such as #7119, and call an ambulance without hesitation if necessary.
- At the same time, vaccination against COVID-19 and seasonal influenza of those who are subject to vaccination should be promoted.
- 6. Surveillance and risk assessment, etc.
- It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status. It is also necessary to continue monitoring of the trends of variants through genomic surveillance.
- Regarding the risk assessment of COVID-19, it is necessary to continue evaluation of the pathogenicity, infectivity, mutations, etc.
- 7. Effective ventilation
- It is necessary to publicize and recommend effective ventilation methods to prevent insufficient indoor ventilation (how to create airflow considering aerosols and installation of partitions that do not block the airflow, for example) due to the use of heating appliances due to low temperatures.
- 8. Re-inspection and implementation of basic infection control measures
Re-inspection and implementation of the following basic infection control measures are needed.
- Continue proper wearing of nonwoven masks according to the situation, hand hygiene, thorough ventilation, etc.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, and loud voices.
- In the event of a meeting at a restaurant, choose a venue certified by a third party, keep the number of people as low as possible, avoid speaking in loud voices and staying for a long time, and wear a mask when talking.
- People with symptoms such as sore throat, cough, and fever should refrain from going out.
- Refer to the guidelines for hospital visits and the use of an ambulance.
- Prepare antigen qualitative test kits and antipyretic analgesics at home, and check the contact information of consultation services.
- Make efforts such as promoting the use of telework in the workplace.
- The organizers of events or meetings should examine and evaluate the epidemic status in the concerned region as well as the risk of infection, and then take measures to reduce the risk.
- From March 13 this year, the government will not uniformly request masks as a rule, but will respect the independent choice of individuals, and leave the use of masks to their judgment. Until then, actions will be taken according to the previous policy.
- Test-positive persons on home care should monitor their own physical condition by such means as checking their body temperature, and take thorough measures against infection when going out. They must also be asked to avoid contact with people who are at risk of severe disease, such as elderly people.
- After 24 hours have passed since symptoms have subsided or when there are no symptoms, in allowing the minimum necessary outings such as shopping for groceries, it is necessary to take voluntary actions to prevent infection, such as wearing a mask when going out, keeping contact with other people at the minimum period of time possible, and not using public transportation.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is also considered to have occurred via droplets adhering to mucosa, aerosol inhalation, contact infection, etc.
- [Severity, etc.]
It has been shown that infection with the Omicron variant may present a relatively lower risk of hospitalization or aggravation than with the Delta variant. To evaluate COVID-19, including the Omicron variant, it is not only necessary to assess the severity as a disease but also of the transmissibility and the impact on the medical care system and society as a whole.
Concerning the death toll since the outbreak at the end of 2021, it is reported that the novel coronavirus is not the direct cause of death in quite a number of cases compared to the epidemic in the summer of 2021; for example, when elderly people who had been living in a facility for elderly people since before the infection were infected and died, the death was due to worsening of the underlying disease. There were many cases of serious respiratory failure due to typical viral pneumonia caused by the novel coronavirus infection from the beginning of the novel coronavirus outbreak until the outbreak of the Delta variant. However, during the Omicron variant outbreak, it was reported that other diseases than pneumonia became the main causes of death, such as exacerbation of the underlying disease that had been present before hospitalization and the onset of other complications during hospitalization.
Concerning the spread of infection last summer, there has been a continuing decrease in the rate of severe cases and increase in the ratio of elderly people among hospitalized patients as during the previous outbreak compared to spreading of the infection in the summer of 2021. Among the deaths during the 2022 summer outbreak, mechanical ventilation/nasal high flow use rates and steroid prescription rates were decreased compared to the end of 2021 outbreak.
Among the fatal cases of infected children who died of endogenous factors, there were some cases without any underlying diseases. The reports on the results of on-site investigations have stated that it is necessary to pay attention to neurological symptoms such as convulsions and disturbance of consciousness, and systemic symptoms such as vomiting and poor oral intake besides the respiratory symptoms.
Among the deaths that occurred at home in July and August last year, approximately 80% of the patients were 70 years and older, which is similar to the trend of all deaths during the same period. It suggests that there were also many deaths caused by factors other than COVID-19. Regarding the situation of handling dead bodies known to be coronavirus positive, the number of cases reported monthly has been the highest during last December. The proportion of deaths due to COVID-19 has recently reached approximately 30% of all deaths.
- [Virus shedding period]
According to Japanese data, the risk of infection remains until 10 days after the onset, and infectivity is high until 7 days after the onset. Even after waiting for 5 days, a third of the patients are still shedding infectious viruses. On Day 8 (after isolation for 7 days), most patients (approximately 85%) did not shed infectious viruses, and it was reported that even if patients did shed the virus, the amount of virus decreased to one-sixth that in the initial stage of onset after 7 days.
- [Vaccine effects]
Concerning the conventional vaccine, the infection and disease onset prevention effects of the first vaccination against the Omicron variant are markedly reduced. The hospitalization-preventing effect is reported maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing, disease onset-preventing and hospitalization-preventing effects against infection with the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Concerning the vaccine against the Omicron variant (BA.4-5), it has been reported that the preventive effect against disease onset was observed within 0 to 2 months (median 1 month) after vaccination.
- [Sublineages of the Omicron variant]
While the BA.5 lineage continues to be mainstream in the world, there are reports of sublineages of the Omicron variant and recombinants of them with characteristic mutations in the spike protein. They include sublineages of which a predominance in the increasing number of infected patients has been indicated, such as the BQ.1 lineage (sublineage of the BA.5.3 lineage), the XBB lineage (recombinant of the BJ.1 lineage [sublineage of the BA.2.10 lineage] and the BM.1.1.1 lineage [sublineage of the BA.2.75.3 lineage]), and the CH.1.1 lineage (sublineage of the BA.2.75.3 lineage). The proportion of the BQ.1 lineage has increased in Europe, and it is also increasing in Japan. In addition, the XBB.1.5 lineage (sublineages of the XBB lineage) is on an increasing trend in the US. The World Health Organization (WHO), etc., pointed out that the immune escape of these variants probably leads to dominance in the increasing number of infected cases, but the information obtained so far suggest that there is limited epidemiological and clinical knowledge of the infectivity and severity of the XBB.1.5 lineage. There are also no clear findings on the BN.1.2 and BN.1.3 lineages, which have been increasing in Japan. It is necessary to continue to collect data and analyze the situation and findings in other countries regarding these characteristics of the new sublineages and recombinants, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)
- Details
116th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (February 8, 2023) Material 1
Evaluation of the latest infection status, etc.
Overview of the infection status, etc.
- The number of new cases of infection nationwide was approximately 214 per 100,000 of the population in the last week, showing a continuous decreasing trend with a ratio of this week to last week of 0.72.
It is necessary to pay attention to the future impact of attenuation of immunity and replacement by variant strains on the infection status. - The use rate of beds has been decreasing nationwide, and the number of deaths and emergency cases that are difficult to transport have also continued to decrease although the numbers remain high.
Reference: Local trend
* The number of new cases of infection is an approximate figure per 100,000 of the population, as the total for the current week, which is the reported number in HER-SYS as of Feb. 7, 00:00 AM (the same time point is used for the ratio to the previous week), and the use rate of beds is the secured bed use rate as of the time of writing this document on Feb. 7.
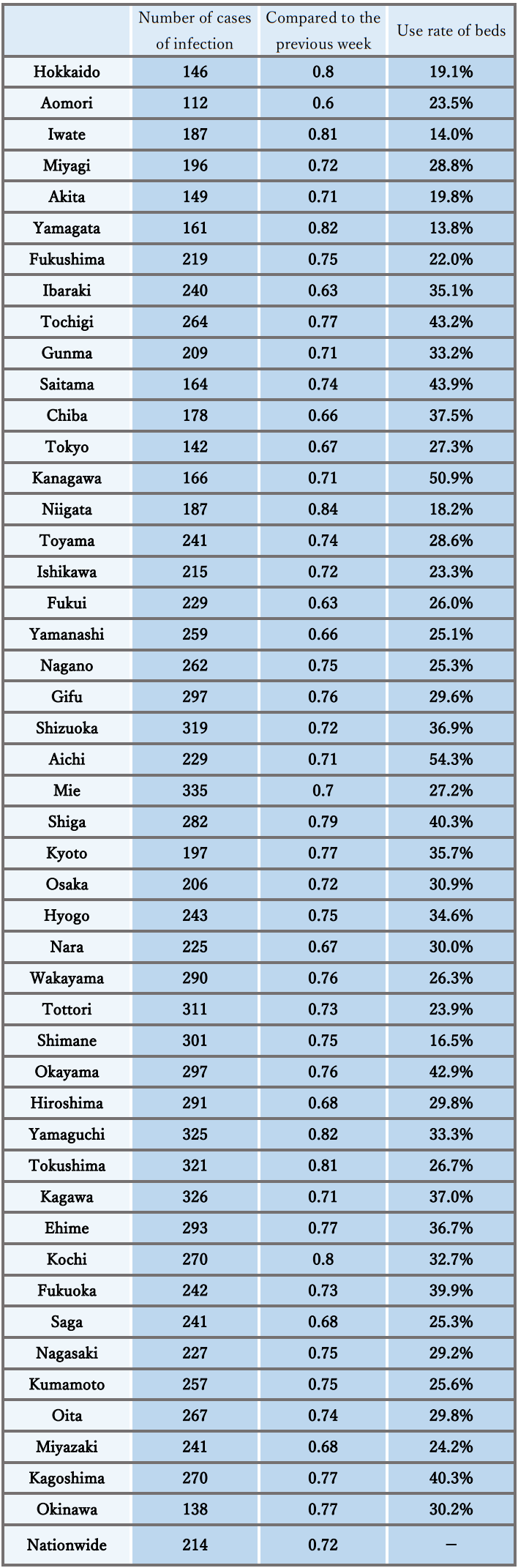
Infection status and future outlook
Infection status
- The number of new cases of infection shows a continuous decreasing trend nationwide, and the ratio to the previous week remains below 1.0 in all prefectures.
- Regarding the number of new cases of infection by region, in the Tokai, Chugoku, Shikoku, and Kyushu regions, the number per population is higher than the national average. Meanwhile, in the Hokkaido, Tohoku and Kanto regions and Okinawa, the number is lower than the average. However, the regional differences are also decreasing as the infection status improves. In addition, there is a decreasing trend in mass infections in facilities for elderly people, medical institutions, etc.
- The number of new cases of infection nationwide by age group shows a decreasing trend in all age groups. A decrease in the number is significant even in the group of those under 10 years old that accounts for a large proportion of new cases of infection.
- The number of severe cases has been decreasing nationwide, and the number of deaths has also continued to decrease, although the number remains high. With the recent expansion of infection, the proportion of elderly patients in their 80s and older among newly infected patients shows an increasing trend compared to that at the time of expansion of the infection the last summer. Attention should continuously be paid because the underlying diseases tend to deteriorate in winter.
- As the reports of deaths among children since January 2022 suggest, attention must be paid to the occurrence of severe cases and deaths as well as the number of hospitalized children associated with an increase in the number of infected children.
- The incidence of seasonal influenza is lower than during the same period in usual years, but higher than during the same period in the previous two years. At the time of the announcement last weekend, the number of cases reported weekly per fixed-point medical institution exceeded 10 nationwide, and the number exceeded 30 in Okinawa. Both numbers have reached a warning level. Nationwide, the number is still on an increasing trend, although the increase is smaller than in the previous week.
Future outlook
- Regarding the future infection status, it is expected to show a continuous decreasing trend nationwide, despite regional differences and uncertainty, based on the epi curves and short-term forecasts nationwide and in large cities. It is necessary to pay attention to the future impact of the attenuation of immunity and an increase in the proportion of strains with the ability to escape the immune system on the infection status.
- Concerning the level of seasonal influenza, an increase in infection cases is expected to continue based on past trends, although the increase is narrowing. Attention needs to be paid to simultaneous infection of influenza and COVID-19.
Factors that increase and suppress infection
- [Immunity as a result of vaccination and infection]
With the promotion of vaccination and natural infection, the proportion of immune carriers against the Omicron variant (BA.5 and BQ1.1) shows an increase in each age group, and it has been reported that the percentage is increasing particularly in the elderly population as a result of vaccination. However, immunity acquired both through vaccination and natural infection is considered to decrease over time, and it may already have declined in elderly people.
- [Contact situation]
The nighttime population has recently increased in many large cities but has decreased in some regions, showing regional differences.
- [Epidemic strains]
Currently, the BA.5 lineage is the mainstream in Japan, but sublineages of the Omicron variant such as BQ.1 and XBB lineages, particularly XBB.1.5, which has been reported mainly in the US, are considered to have an enhanced ability to escape the immune system, and have been pointed out to predominate among the increasing number of infected people overseas. Particularly regarding the BQ.1 lineage, the proportion is increasing domestically, and close attention is required. The proportion of BN.1.2 and BN.1.3 lineages, which are sublineages of the BA.2.75 lineage, has also increased in Japan.
- [Climatic and seasonal factors]
With a full-fledged winter, temperatures are dropping nationwide, and ventilation may be difficult. Respiratory virus infections also tend to be prevalent in winter.
Situation of the medical care provision system
- The use rate of beds has been decreasing nationwide and is below 50% in almost all regions. The use rate of beds for severe cases has also been declining in many regions.
- The number of patients receiving treatment in nursing care facilities has been decreasing.
- As for emergency medical care, while the medical care system is usually overloaded in winter, the number of cases having difficulty with emergency transportation remains at a high level nationwide but shows a continuous decreasing trend. Attention should continuously be paid to the future trend of the number of cases having difficulty with emergency transportation and securing a system to provide emergency medical care.
Measures to be taken
Basic concepts
- Unless we face special circumstances such as the emergence of a variant with a pathogenicity greatly different from that of the Omicron variant, COVID-19 shall be positioned as a Class V Infectious Disease instead of a Novel Influenza Infection, etc. under the Infectious Disease Act from May 8 this year (2023). In association with this, various policies and measures taken will be reviewed.
- Meanwhile, it is necessary to continue efforts to strengthen and focus the healthcare system to provide appropriate medical care for elderly people and those at high risk of aggravation, even with limited medical resources.
Each citizen will be asked to take voluntary actions to prevent infection to protect those at high risk of aggravation, such as elderly people, and to ensure regular medical care.
- 1. Further promotion of vaccination
- As for the “vaccine for the Omicron variant," vaccination of all persons aged 12 and over who have completed the first vaccination should proceed.
- As both vaccines for the BA.1 and the BA.4 and BA.5 lineages are expected to be more effective than the previous vaccines, it is necessary to proceed with vaccination with the vaccine that can be given sooner. All eligible persons who wish to receive vaccination will be asked to receive the vaccine for the Omicron variant.
- Those who have not received vaccination will be encouraged to consider getting the initial vaccination as soon as possible.
- For children (ages 5 to 11), booster vaccinations will be promoted along with the initial vaccination. For children (ages 6 months to 4 years), initial vaccinations will be promoted.
- It is necessary to discuss promptly how to position the coronavirus vaccination in the future.
- 2. Use of tests
- The national and local governments are required to secure a system that enables testing, and should utilize testing.
- Perform frequent tests (about 2 or 3 times a week for facility workers) for workers at facilities for elderly people.
- Promote the establishment of a system for fever outpatients, whereby patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Promote the utilization of antigen qualitative test kits, which have been switched to OTC and are sold on the internet.
- 3. Quarantine measures
- The COVID-19 situation in China is rapidly worsening, making it difficult to grasp the details. Based on this situation, temporary measures such as immigration inspections have been implemented since December 30, 2022 to avoid a sharp increase in the inflow of COVID-19 into Japan, and flexible responses will be taken while monitoring the infection situation in China.
- 4. Securing a medical care provision system
- In winter, it is also the time when the number of patients with other diseases than COVID-19 increase. With the support of the national government, prefectural governments must take measures mainly to avoid overcrowding of hospital beds and fever outpatient clinics.
- Maintain the total number of beds required for patients infected with COVID-19 based on the bed securing plan. In addition, continue to increase the number of medical institutions that can handle COVID-19 by supporting improvement of the ability to treat COVID-19 cases, even at hospitals without any beds for infected patients (promotion of zoning of hospital rooms, etc.).
- Take immediate responses such as securing beds, and make efforts to avoid being overwhelmed concerning the number of hospital beds and emergency medical care by using lodging facilities and resting beds, for example.
- Make appropriate adjustments so that patients who need hospital treatment can be hospitalized preferentially (securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule). Implement frequent examinations at facilities for elderly people and others. Further strengthen medical support during normal times.
- In addition to extending the office hours and the number of outpatient clinics for fever patients, the outpatient medical care system is strengthened and prioritized by strengthening regional outpatient and testing centers and telephone and online clinics, etc.
- Local residents should be informed that they should refrain from visiting emergency outpatient units only to receive a precautionary examination if they do not have symptoms, for example, taking the actual situation in the region into consideration, so that nobody is prevented from receiving treatment. To respond to concerns and questions when a patient’s physical condition deteriorates, the telephone consultation service by healthcare professionals should be thoroughly publicized, and this service should also be strengthened.
- Ensuring that workplaces and schools do not require test certificates at the start of medical treatment
- 5. Response to simultaneous epidemics of COVID-19 and seasonal influenza
- As measures for people with fever during simultaneous epidemics, the following efforts should be promoted according to the actual situation in each region: strengthening of the fever outpatient clinics, strengthening of telephone consultations/telemedicine, expansion of health follow-up centers, securing of self-test kits, strengthening of the consultation system, and prevention of overcrowded emergency medical care.
Smooth supply of medications including oral drugs prescribed after confirmation of the indication by physicians will be promoted. Pharmacies, etc. will be asked to use the consultation service of the Ministry of Health, Labour and Welfare when it is difficult to obtain antipyretic analgesics. - The prefectures will work to strengthen and prioritize the health care system based on plans to establish systems such as strengthening of outpatient medical care systems in accordance with the actual conditions in each region.
- It is necessary to provide information and appropriate messages depending on the infection status to the public. People at low risk of aggravation will be encouraged to use a self-test kit or local follow-up center. People will be advised to do the following: check the “guide for ambulance services” in preparation for an acute illness or injury, consult a family doctor when hesitant to call an ambulance, use a telephone consultation service such as #7119, and call an ambulance without hesitation if necessary.
- At the same time, vaccination against COVID-19 and seasonal influenza of those who are subject to vaccination should be promoted.
- As measures for people with fever during simultaneous epidemics, the following efforts should be promoted according to the actual situation in each region: strengthening of the fever outpatient clinics, strengthening of telephone consultations/telemedicine, expansion of health follow-up centers, securing of self-test kits, strengthening of the consultation system, and prevention of overcrowded emergency medical care.
- 6. Surveillance and risk assessment, etc.
- It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status. It is also necessary to continue monitoring of the trends of variants through genomic surveillance.
- Regarding the risk assessment of COVID-19, it is necessary to continue evaluation of the pathogenicity, infectivity, mutations, etc.
- 7. Effective ventilation
- It is necessary to publicize and recommend effective ventilation methods to prevent insufficient indoor ventilation (how to create airflow considering aerosols and install partitions that do not block airflow, for example) due to the use of heating appliances due to low temperatures.
- 8. Re-inspection and implementation of basic infection control
Re-inspection and implementation of the following basic infection control measures are needed.
- Continue proper wearing of nonwoven masks according to the situation, hand hygiene, thorough ventilation, etc.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, or loud voices.
- In the event of a meeting at a restaurant, choose a venue certified by a third party, keep the number of people as low as possible, avoid speaking in loud voices and staying for a long time, and wear a mask when talking.
- People with symptoms such as sore throat, cough, and fever should refrain from going out.
- Refer to guidelines for hospital visits and use of an ambulance.
- Prepare antigen qualitative test kits and antipyretic analgesics at home, and check the contact information of consultation services.
- Make efforts such as promoting the use of telework in the workplace.
- The organizers of events or meetings should examine and evaluate the epidemic status in the concerned region as well as the risk of infection, and then take measures to reduce the risk.
- Test-positive persons on home care should monitor their own physical condition by such means as checking their body temperature and taking thorough measures against infection when going out. They must also be asked to avoid contact with people who are at risk of aggravation, such as elderly people.
- To allow the minimum necessary outings, such as shopping for groceries, after 24 hours have passed since symptoms have subsided or when there are no symptoms, it is necessary to take voluntary actions to prevent infection, such as wearing a mask when going out, keeping contact with other people at the minimum period of time possible, and not using public transportation.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is considered to have occurred via the same routes as before (droplets adhering to the mucosa, aerosol inhalation, contact infection, etc.).
- [Severity, etc.]
It has been shown that infection with the Omicron variant may present a relatively lower risk of hospitalization and aggravation than with the Delta variant. To evaluate COVID-19, including the Omicron variant, it is not only necessary to assess the severity as a disease but also of the transmissibility and the impact on the medical care system and society as a whole.
Concerning the death toll since the outbreak at the end of 2021, it is reported that the novel coronavirus is not the direct cause of death in quite a number of cases compared to the epidemic in the summer of 2021; for example, when elderly people who had been living in a facility for elderly people since before the infection were infected and died, the death was due to worsening of the underlying disease. There were many cases of serious respiratory failure due to typical viral pneumonia caused by the novel coronavirus infection from the beginning of the novel coronavirus outbreak until the outbreak of the Delta variant. However, during the Omicron variant outbreak, it was reported that other diseases than pneumonia became the main causes of death, such as exacerbation of the underlying disease that had been present before hospitalization and the onset of other complications during hospitalization.
Concerning the spread of infection last summer, there has been a continuing decrease in the rate of severe cases and increase in the ratio of elderly people among hospitalized patients as during the previous outbreak compared to spreading of the infection in the summer of 2021. Among the deaths during the 2022 summer outbreak, mechanical ventilation/nasal high flow use rates and steroid prescription rates were decreased compared to the 2021 outbreak.
Among the fatal cases of infected children who died of endogenous factors, there were some cases without any underlying diseases. The reports on the results of on-site investigations have stated that it is necessary to pay attention to neurological symptoms such as convulsions and disturbance of consciousness, and systemic symptoms such as vomiting and poor oral intake besides the respiratory symptoms.
Among the deaths that occurred at home in July and August last year, approximately 80% of the patients were 70 years and older, which is similar to the trend of all deaths during the same period. It suggests that there were also many deaths caused by other factors than COVID-19. Regarding the situation of handling dead bodies known to be coronavirus positive, the number of cases reported monthly has been the highest during last December. The proportion of deaths due to COVID-19 has recently reached approximately 30% of all deaths. The local governments are developing outpatient medical care and health follow-up systems including medical institutions that provide care or perform examinations. It is important to continuously endeavor to provide the necessary medical care to home care patients.
- [Virus shedding period]
According to Japanese data, the risk of infection remains until 10 days after the onset, and infectivity is high until 7 days after the onset. Even after waiting for 5 days, a third of the patients are still shedding infectious viruses. On Day 8 (after isolation for 7 days), most patients (approximately 85%) did not shed infectious viruses, and it was reported that even if patients did shed the virus, the amount of virus decreased to one-sixth that in the initial stage of onset after 7 days.
- [Vaccine effects]
Concerning the conventional vaccine, the infection and disease onset prevention effects of the first vaccination against the Omicron variant are markedly reduced. The hospitalization-preventing effect is reported maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing, disease onset-preventing and hospitalization-preventing effects against infection with the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Concerning the vaccine against the Omicron variant (BA.4-5), it has been reported that the preventive effect against disease onset was observed within 0 to 2 months (median 1 month) after vaccination.
- [Sublineages of the Omicron variant]
While the BA.5 lineage continues to be mainstream in the world, there are reports of sublineages of the Omicron variant and recombinants of them with characteristic mutations in the spike protein. They include sublineages of which a predominance in the increasing number of infected patients has been indicated, such as the BQ.1 lineage (sublineage of the BA.5.3 lineage), the XBB lineage (recombinant of the BJ.1 lineage [sublineage of the BA.2.10 lineage] and the BM.1.1.1 lineage [sublineage of the BA.2.75.3 lineage]), and the CH.1.1 lineage (sublineage of the BA.2.75.3 lineage). The proportion of the BQ.1 lineage has increased in Europe, and it is also increasing in Japan. In addition, the XBB.1.5 lineage (sublineages of the XBB lineage) is on an increasing trend in the US. The World Health Organization (WHO), etc., pointed out that the immune escape of these variants probably leads to dominance in the increasing number of infected cases, but the information obtained so far suggest that there is limited epidemiological and clinical knowledge of the infectivity and severity of the XBB.1.5 lineage. There are also no clear findings on the BN.1.2 and BN.1.3 lineages, which have been increasing in Japan. It is necessary to continue to collect data and analyze the situation and findings in other countries regarding these characteristics of the new sublineages and recombinants, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)