Infectious Deseases
Basic Research
Surveillance
Information
- Details
103rd Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (October 20, 2022) Material 1
Evaluation of the latest infection status, etc.
Overview of the infection status
- Nationwide, the number of new cases of infection (by date of report) was approximately 197 per 100,000 in the last week, and ratio to the previous week was 1.35. As the rate has increased, we need to carefully watch the speed of increase and also whether this trend will continue in the future.
It is also necessary to pay attention to the future impact of increased contact opportunities due to the reactivation of socioeconomic activities on the infection status. - In contrast, the use rate of beds is generally on a downward trend, at a low level. The numbers of severe cases and deaths have stopped decreasing.
Local trends
* The value of new cases of infection is the number of persons per 100,000 among the total number for the latest week, based on the reporting dates.
- Hokkaido
The number of new cases of infection was approximately 397 (approximately 355 in Sapporo City), and the ratio to the previous week was 1.60. The use rate of beds is approximately 20%.
- North Kanto
In Ibaraki, Tochigi, and Gunma, the numbers of new cases of infection were approximately 190, 188, and 224, and the ratios to the previous week were 1.47, 1.34, and 1.35, respectively.
The use rates of beds were slightly over 20% in Ibaraki and Gunma, and slightly over 10% in Tochigi. - Tokyo metropolitan area (Tokyo and 3 neighboring prefectures)
The number of new cases of infection in Tokyo was approximately 169, and the ratio to the previous week was 1.25. The use rate of beds was slightly over 10%, while the use rate of beds for severe cases was below 10%.
In Saitama, Chiba, and Kanagawa, the numbers of new cases of infection were approximately 152, 145, and 146, respectively, and the ratios to the previous week were 1.23, 1.20, and 1.16, respectively.
The use rates of beds were approximately 20% in Saitama, slightly under 20% in Kanagawa and slightly over 10% in Chiba. - Chukyo/Tokai
The number of new cases of infection in Aichi was approximately 151, and the ratio to the previous week was 1.28. The use rate of beds was slightly over 20%.
In Gifu, Shizuoka, and Mie, the numbers of new cases of infection were approximately 249, 191, and 217, and the ratios to the previous week were 1.46, 1.43, and 1.45, respectively.
The use rates of beds were slightly over 10% in Gifu, slightly under 20% in Shizuoka, and approximately 20% in Mie. - Kansai area
The number of new cases of infection in Osaka was approximately 205, and the ratio to the previous week was 1.40. The use rate of beds was slightly over 10%, while the use rate of beds for severe cases was below 10%.
In Shiga, Kyoto, Hyogo, Nara, and Wakayama, the numbers of new cases of infection were approximately 220, 133, 157, 191, and 282, and the ratios to the previous week were 1.33, 1.22, 1.49, 1.47, and 1.75, respectively.
The use rates of beds were slightly over 20% in Shiga, approximately 20% in Wakayama, and slightly over 10% in Hyogo, Kyoto and Nara. - Kyushu
The number of new cases of infection in Fukuoka was approximately 153, and the ratio to the previous week was 1.38. The use rate of beds was approximately 10%.
In Saga, Nagasaki, Kumamoto, Oita, Miyazaki, and Kagoshima, the numbers of new cases of infection were approximately 178, 148, 186, 188, 169, and 134, and the ratios to the previous week were 1.33, 1.25, 1.28, 1.41, 1.26, and 1.01, respectively. The use rates of beds were slightly over 10% in Kumamoto, Oita, and Kagoshima, approximately 10% in Nagasaki and Miyazaki, and slightly under 10% in Saga. - Okinawa
The number of new cases of infection was approximately 132, and the ratio to the previous week was 0.85. The use rate of beds was approximately 10%, and the use rate of beds for severe cases was slightly under 10%.
- Other areas than the above
In Iwate, Yamagata, Toyama and Kagawa the ratios to the previous week were 1.53, 1.56, 1.51, and 1.60, respectively. The use rates of beds were slightly over 20% in Aomori, Akita, Fukushima, Ishikawa, Nagano and Hiroshima.
Infection status and future outlook
Infection status
- Nationwide, the number of new cases of infection increased and the ratios to the previous week in almost all regions are higher than 1. We need to carefully watch the speed of increase as well as whether this trend will continue in the future. It is also necessary to consider the effect of consecutive holidays in the last week. The numbers of new cases of infection have increased in many regions of northern Japan. There are also still mass infections in some facilities for elderly people and medical institutions.
- The number of new cases of infection by age group increased in almost all age groups, and new patients per population were higher in younger age groups. The number of new cases of infection among elderly people also increased, and the numbers of severe cases and deaths stopped decreasing.
- As the provisional report of deaths among children since January this year suggests, attention must be paid to the occurrence of severe cases and deaths associated with an increase in the number of infected children.
Future outlook
- Regarding the future infection status, the number of infections may continue to increase despite uncertainty, based on the short-term forecast in large cities. It is also necessary to pay attention to the future impact of increased contact opportunities due to the reactivation of socioeconomic activities on the infection status.
- Based on the estimated trends of the past two years, there is concern about earlier spread of the new coronavirus infection this winter, an earlier seasonal flu epidemic than usual, which is at a low level at this point, and that these two may occur simultaneously.
Factors that increase and suppress infection
- [Immunity as a result of vaccination and infection]
Immunity acquired from vaccination and natural infection may decline over time. Although the vaccination rate is higher among people in their 60s and older than those in their 20s to 40s, the acquisition of immunity by infection is lower, and there is concern about the spread of infection among elderly people.
- [Contact patterns]
The nighttime population is increasing in many regions. There is also a concern that the nighttime population will further increase toward the end of the year.
- [Epidemic strain]
In Japan, the BA.5 lineage has largely become mainstream, and is replacing others. At present, there is not a trend toward further replacement by other lineages.
- [Climatic factors]
Weather conditions will be favorable for ventilation for a while, but ventilation may be difficult on days with a low temperature or bad weather such as heavy rainfall.
Situation of the medical care provision system
- Nationwide, the use rate of beds is generally decreasing and the rates in all areas are at a low level below 30%. The use rate of beds for severe cases is also at a low level, but we need to watch for effects associated with an increase in the number of new cases of infection.
- In the field of nursing care, patients are being treated in the facilities and infections are seen among workers.
- Cases of problems with emergency transportation remain on the same level nationwide both for suspected non-COVID-19 cases and suspected COVID-19 cases.
Measures to be taken
Basic concepts
- To prepare for re-spreading of the novel coronavirus infection and simultaneous seasonal influenza epidemics, measures to strengthen and focus the healthcare system should be taken for limited medical resources to provide appropriate medical care to elderly people and persons at risk of aggravation.
- Each citizen will be asked to take voluntary actions to prevent infection and strengthening and prioritization of the health care system will be promoted to protect those at high risk of aggravation, such as elderly people, and to ensure regular medical care.
- The national and local governments will remind the public of the need for routine infection control measures and take measures to support the public's efforts to prevent infection.
- 1. Further promotion of vaccination
- As for the “vaccine for the Omicron variant," vaccination of all persons aged 12 and older who have completed the first vaccination should proceed.
- Vaccination for the BA.4 and BA.5 lineage has also started. As both vaccines for the BA.1 and for the BA.4 and BA.5 lineages are expected to be more effective than the previous vaccines, it is necessary to proceed with vaccination with vaccines that can be given sooner. As the vaccination interval from the last vaccination was shortened from 5 months to 3 months, all eligible persons will be asked to receive the vaccine for the Omicron variant during this year.
- Those who have not received vaccination will be encouraged to consider getting the initial vaccination as soon as possible.
- For children (ages 5 to 11), booster vaccinations will be promoted along with the initial vaccination.
- The initial vaccination for children (aged 6 months to 4 years) has been approved by the PMDA and is positioned as an extraordinary vaccination, and initial vaccination in this age group will proceed.
- 2. Use of tests
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, the national and local governments are required to secure a system that enables testing, and should further utilize testing.
- Performance of frequent tests (about 2 or 3 times a week for facility workers) for workers at facilities for elderly people.
- Further promotion of the establishment of a system whereby patients with symptoms can self-test using an antigen qualitative test kit, and can then promptly undergo health observation at a health follow-up center, etc. if the result is positive.
- Further promotion of the utilization of antigen qualitative test kits that are switched to OTC and are sold on the internet.
- 3. Securing a medical care provision system
Prefectural governments must take measures to avoid overcrowding of beds and fever outpatient clinics with the support of the national government.
- In addition to facilitating the use of available hospital beds and developing temporary medical facilities to supplement hospital beds, making efforts to avoid a shortage of hospital beds and emergency medical care, such as utilization of lodging facilities and resting beds
- Making appropriate adjustments so that patients requiring inpatient treatment can be hospitalized preferentially, performing frequent tests at facilities for elderly people, etc., and further strengthening medical support
- Securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule
- Promotion of effective and less burdensome measures against infection, such as flexible and efficient use of hospital beds through zoning of each hospital room
- Expansion and promotion of fever outpatient services, including the use of online medical care, etc., and further promotion of the development of a “fever outpatient self-examination system”
- Local residents should be informed that they should refrain from visiting an emergency outpatient unit only to receive a precautionary examination without symptoms, according to the actual situation in the region. In addition, in order to respond to concerns and questions at the time of worsening physical conditions, the consultation service by healthcare professionals via telephone should be thoroughly publicized, and this service should also be strengthened.
- Ensuring that workplaces and schools do not require test certificates at the start of medical treatment
- 4. Response to simultaneous epidemics of novel coronavirus infection and seasonal influenza
- Assuming that there are many patients with fever during simultaneous epidemics, the following measures should be promoted according to the actual situation of each region: strengthening of fever outpatient clinics, strengthening of telephone and online examination services in preparation for cases of overcrowding at fever outpatient clinics, smooth supply of therapeutic drugs, expansion of health follow-up centers, securing of self-examination kits, and strengthening of the consultation system.
- The prefectures will formulate plans to establish systems such as strengthening of outpatient medical care systems in accordance with the actual conditions in each region.
- In addition, efforts will be made to provide information to the public and to call for cooperation at clinic visits/treatment according to the risk of aggravation.
- To prevent the infection from becoming severe as far as possible when symptoms occur, vaccination against the new coronavirus and influenza virus should also be promoted among those to be vaccinated.
- In case the number of infected persons increases extremely and hospitals are under severe strain, or changes in the characteristics of viruses increase the pathogenicity, a response depending on the situation is required, and includes requests/calls for residents and business operators to prevent spreading of the infection and to maintain the functions of medical systems, as well as highly effective measures to prevent the spread of infection including behavioral restrictions.
- 5. Surveillance
- The limited scope of notification of occurrence, notified items, delay in testing/diagnosis/reporting due to the many cases of the infection, changes in medical care-seeking behavior, etc. are raising concerns about deterioration of the current surveillance program’s accuracy. To understand the epidemiological status, an effective and appropriate surveillance program should be developed promptly.
It is also necessary to continue monitoring the trends of variants through genomic surveillance.
- The limited scope of notification of occurrence, notified items, delay in testing/diagnosis/reporting due to the many cases of the infection, changes in medical care-seeking behavior, etc. are raising concerns about deterioration of the current surveillance program’s accuracy. To understand the epidemiological status, an effective and appropriate surveillance program should be developed promptly.
- 6. Effective ventilation
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, it is necessary to publicize and recommend effective ventilation methods to prevent insufficient indoor ventilation (how to create airflow considering aerosols, installation of partitions that do not block airflow, etc.).
- 7. Re-inspection and implementation of basic infection control
Re-inspection and implementation of the following basic infection control measures are necessary.
- Continue proper wearing of nonwoven masks according to the situation, hand hygiene, thorough ventilation, etc.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, or loud voices.
- Eating and drinking should be done with as few people as possible, and masks should be worn except while eating and drinking.
- People with symptoms such as sore throat, cough, and fever should refrain from going out.
- Refer to guidelines for hospital visits and use of an ambulance.
- To reduce the chances of contact as far as possible, measures are necessary at the workplace are needed, such as and include again promoting the use of telework.
- Organizers of events, meetings, etc., should fully evaluate the epidemic situation and risk of infection in the area, and consider whether or not to hold the gathering, and if it is held, measures should be taken to minimize the infection risk.
- Since a risk of infection remains during the shortened period of home care of those who test positive, they should monitor their own physical condition, such as measuring their temperature, and take thorough measures against infection when going out. They must also be asked to avoid contact with people who are at risk of aggravation, such as elderly people.
- To allow the minimum necessary outings, such as shopping for groceries, after 24 hours have passed since symptoms have subsided or when there are no symptoms, it is necessary to take voluntary actions to prevent infection, such as wearing a mask when going out or when having contact with people, keeping contact with people to a minimum period of time, and not using public transportation.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is considered to have occurred via the same routes as before (droplets adhering to mucosa, aerosol inhalation, contact infection, etc.).
- [Severity]
It has been suggested that infection with the Omicron variant presents a lower risk of hospitalization or aggravation than the Delta variant. However, analyses to date show that the fatality due to infection with the Omicron variant is higher than that due to seasonal influenza. It is also suggested that the incidence of pneumonia is higher than that of seasonal influenza, but given the limited data, it needs to be investigated by various analyses.
In the death toll from the previous outbreak compared to last summer‘s outbreak, it is reported that there are many cases in which the new coronavirus infection is not the direct cause of death, for example, people who have been in a facility for the elderly before the infection are infected and die due to the worsening of the underlying disease. In the current spread of infection, the rate of severe cases has continued to decrease and the ratio of elderly people among hospitalized patients has increased compared to the previous summer, following the previous outbreak. Among the deaths in this outbreak, mechanical ventilation/nasal high flow use rates and steroid prescription rates have decreased compared to the previous outbreak.
Among fatal cases in which endogenous death was identified in infected children, cases without underlying diseases were also found. Preliminary reports on the results of on-site investigations have stated that it is necessary to pay attention to neurological symptoms such as convulsions and disturbance of consciousness, and systemic symptoms other than respiratory symptoms such as vomiting and poor oral intake.
- [Virus shedding period]
According to Japanese data, risk of infection remains until 10 days after onset, and infectivity is high until 7 days after onset. Even after waiting for 5 days, 1/3 of patients are still shedding infectious viruses. On Day 8 (after waiting 7 days), most patients (approximately 85%) had not shed infectious virus, and it was reported that even in those who shed the virus, the amount of virus decreased to one-sixth after 7 days compared to the initial stage.
- [Vaccine effect]
For infection with the Omicron variant, the preventive effects of a first vaccination against infection and disease onset are markedly reduced. Its preventive effect on hospitalization is reported to be maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing effect, onset-preventing effect, and hospitalization-preventing effect against infection by the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Regarding the fourth vaccination, it has been reported that while the preventive effect against aggravation was not reduced for 6 weeks, the preventive effect against infection lasted only for a short time.
- [Sublineages of the Omicron variant]
While the BA.5 lineage continues to be mainstream in the world, there are many reports of sublineages of the Omicron variant and recombinants which have characteristic mutations in the spike protein. There are also sublineages for which superiority in an increase in infected patients has been indicated, including the BQ.1 and BQ.1.1 lineages (sublineages of the BA.5.3 lineage), which are frequently reported in Europe and the United States, as well as the XBB lineage (recombinant of the BJ.1 lineage [sublineages of the BA.2.10 lineage] and the BM.1.1.1 lineage [sublineages of the BA.2.75.3 lineage]), which has been reported mainly in India and Singapore. In particular, in the United States, there is concern that the proportion of the BQ.1 and BQ.1.1 lineages will increase in the future. However, no clear findings of infectivity and severity, etc. of these variants have been obtained. It is necessary to continue to collect and analyze the situation and findings in other countries regarding these characteristics of the new sublineages and recombinants, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)
- Details
Published: October 26, 2022
Center for Field Epidemic Intelligence, Research and Professional Development,
National Institute of Infectious Diseases
Center for Surveillance, Immunization, and Epidemiologic Research,
National Institute of Infectious Diseases
We would like to express our deepest condolences to the bereaved families of all those who have passed away after SARS-CoV-2 infection.
Background and objectives
The Ministry of Health, Labour, and Welfare (MHLW) requested local public health authorities to conduct genome analysis of severe and fatal cases of SARS-CoV-2 infection to accumulate and monitor knowledge on the severity of SARS-CoV-2 infection on the basis of “the enhanced field epidemiological investigation requested for conducting genome analysis and variant screening by real-time polymerase chain reaction (PCR) tests for SARS-CoV-2 (Administrative notice #0205-4 from the Director of Tuberculosis and Infectious Disease Control Division, Health Serviced Bureau of MHLW on February 5, 2021; partially revised on February 10, 2022)” and “Regarding the handling of hospital admissions and discharges, close contacts, and disclosure of patients with confirmed infection by the B.1.1.529 lineage (Omicron variant) (Administrative notice from MHLW on February 2, 2021)” promulgated by Article 15, the Act on the Prevention of Infectious Diseases and Medical Care for Patients with Infectious Diseases (Act No. 114 of October 2, 1998).
Recently, the MHLW and the National Institute of Infectious Diseases (NIID) have been concerned about the severe or fatal pediatric cases of SARS-CoV-2 infection as the number of pediatric cases increased 1), so we conducted an epidemiological investigation of fatal cases of SARS-CoV-2 infection in patients under 20 years old (fatal pediatric cases). Fatal pediatric cases included those caused both directly and indirectly by SARS-CoV-2 infection. We collaborated with three academic societies: the Japan Pediatric Society, the Japanese Society of Intensive Care Medicine, and the Japanese Association for Acute Medicine.
This record is an interim analysis of the fatal pediatric cases reported from January 1 to August 31, 2022.
Methods
Subjects who satisfied either of the following two conditions were included in the investigation. Research staff or fellows of the Field Epidemiology Training Program for NIID collected epidemiological data of local health authorities and visited medical institutions to collect data on medical records if possible and interview physicians (hereafter, field investigation).
Subjects investigated
1)Patients under 20 years old whose date of onset (or admission date) was on January 1, 2022, or later, and who died during the acute phase of infection with SARS-CoV-2.
2)Patients under 20 years old whose date of onset (or admission date) was on January 1, 2022, or later, and who died after the acute phase of infection with SARS-CoV-2 (including cases with other causes of death).
Items investigated
Age, sex, underlying disease, vaccine history of SARS-CoV-2 immunization, date of onset, date of death, symptoms/findings, disease suspected of causing death, and others.
Results (Interim)
A summary of the cases and results of the field investigation as of August 31, 2022, follows below. In collecting the information on the cases, it was difficult to classify the subjects into those exactly meeting criterion 1) or 2). Moreover, we have taken care to ensure that individuals are not identifiable.
〇 Summary of the cases
The total number of cases was 41 (age: <1 year old, n=8 [20%]; 1–4 years old, n=10 [24%]; 5–10 years old, n=17 [41%]; 12–19 years old, n=5 [12%]; and unknown, n=1 [2%]; sex: males, 23 cases [56%] and females, 18 cases [44%]). The figure shows the distribution of cases based on the date of onset after January 1, 2022 (epidemiological week 52, 2021). Cases have been continuously reported since January 2022 and started to increase from epidemiological week 28 (July 11–July 17).
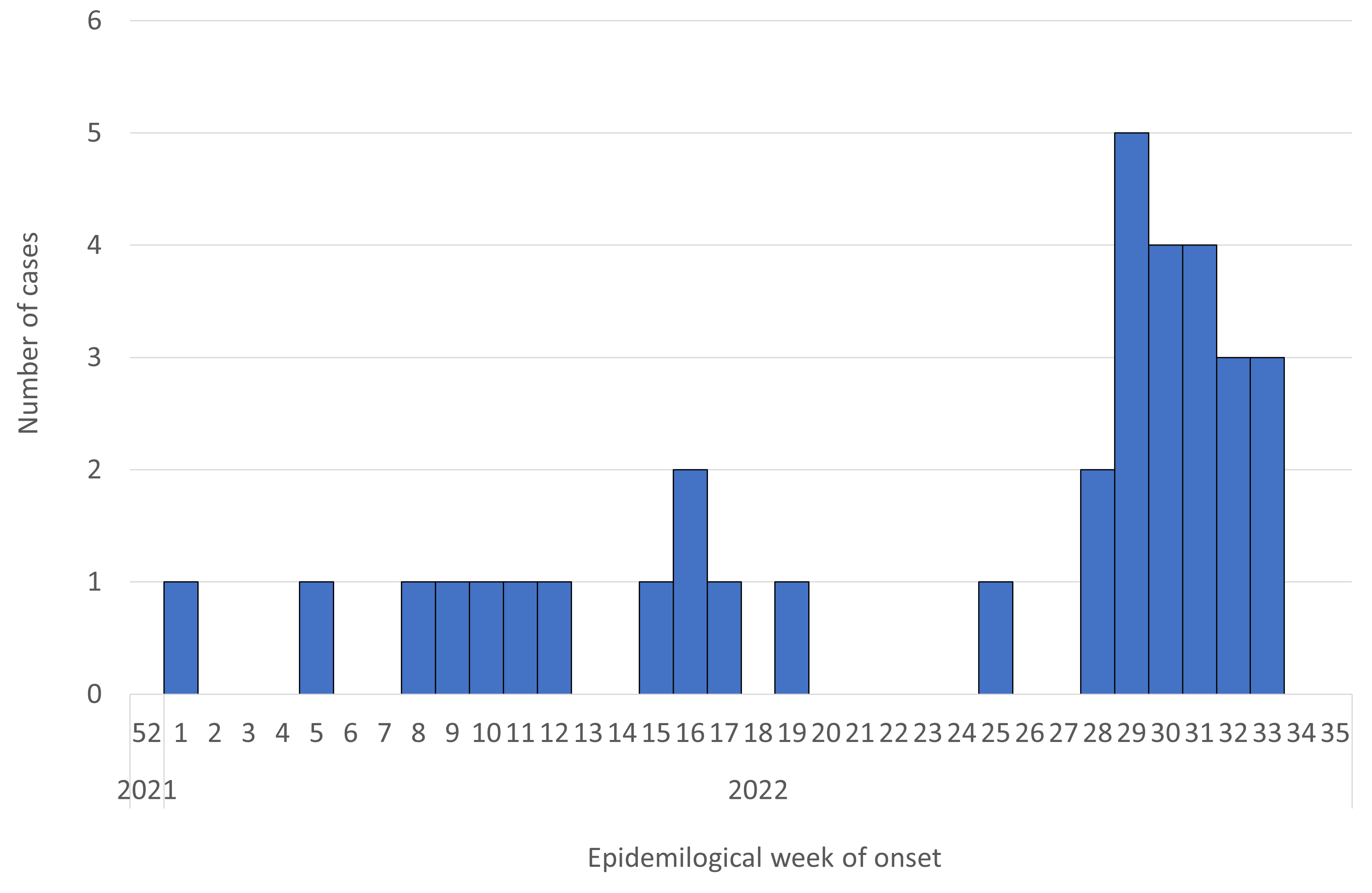
Figure. Reported number of deaths in patients under 20 years of age after SARS-CoV-2 infection (n=34*; date of onset or admission date from January 1, 2022 [week 52, 2021] to August 31, 2022 [week 35, 2022]) (as of August 31, 2022**)
* Seven cases were excluded for unknown date of onset.
** Case numbers in late August may not reflect the actual number of cases due to delayed reporting, so care must be taken in interpreting the data.
〇 Results of the field investigation
Of the 41 cases, we could conduct a field investigation of 32 cases. Among them, 29 cases were considered to be endogenous deaths (death due to other than trauma). The details of these 29 cases are as follows (Table).
Among the 29 cases, eight (28%) patients were <1 year old, six (21%) were 1–4 years old, 12 were 5–11 years old, and three (10%) were 12–19 years old, of whom 16 cases (55%) were in males and 13 cases (45%) were in females. Underlying disease was present in 14 (48%) patients and absent in 15 (52%). As of August 31, 2022, details of underlying disease, including duplicates, showed seven with central nervous system (CNS) abnormalities (50%), two with congenital heart disease (14%), and two with chromosomal abnormalities (14%). Among these 29 patients, 14 (48%) were not eligible for SARS-CoV-2 immunization and 15 (52%) were. Among the 15 patients eligible for SARS-CoV-2 immunization who were 5 years old or older, 13 (87%) were not vaccinated, and two (13%) were vaccinated twice, both of whom were 12 years old or older and whose last vaccination had been more than three months earlier. Moreover, a high number of symptoms or clinical findings on hospital arrival included fever in 23 cases (79%), nausea and/or vomiting in 15 (52%), disturbance of consciousness in 13 (45%), cough in nine (31%), inadequate intake of nutrition in nine (31%), seizure in eight (28%), and dyspnea in seven (24%). The main diseases suspected of causing death in medical institutions included cardiac abnormalities (n=7, 24%: myocarditis, arrhythmia, etc.), CNS abnormalities (n=7, 24%: acute encephalopathy, etc.), respiratory abnormalities (n=3, 10%: pneumonia, bacterial pneumonia, etc.), other diseases (n=6, 21%: multiple organ failure, etc.), and unknown cause of death (n=6, 21%). Several patients with a more rapid disease progression died due to CNS abnormalities such as encephalopathy, etc., and cardiac abnormalities such as myocarditis or arrhythmia. The date of onset was determined in 26 of the 29 cases, and the number of days from onset to death was a median of four days (range: 0–74 days), with eight patients (31%) dying in 0–2 days, 11 dying (42%) in 3–6 days, and seven dying (27%) in 7 days or more.
Of the 29 cases, 14 were thought to have underlying disease, including eight cases (57%) in patients under 5 years old (including four under one year old) and six cases (43%) in patients 6 years old or older. Nine cases (64%) were in males and five cases (36%) were in females. Symptoms or clinical findings on hospital arrival included fever in 11 cases (79%), dyspnea in seven (50%), nausea and/or vomiting in six (43%), cough in five (36%), inadequate intake of nutrition in four (29%), seizure in three (21%), and disturbance of consciousness in three cases (21%). In the medical institutions, the main diseases suspected of causing death were cardiac abnormality (n=3, 21%), respiratory abnormality (n=3, 21%), CNS abnormality (n=2, 14%), other disease (n=3, 21%), and unknown disease (n=3, 21%). Among these 14 cases, date of onset could be obtained in 12, and the number of days from onset to death was a median of four days (range: 1–74 days), with three patients (25%) dying in 0–3 days, seven dying (58%) in 3–6 days, and two dying (17%) in 7 days or more.
Of the 29 cases, 15 were considered to have no underlying disease. These included six cases (40%) in patients under five years old (including four under one year old) and nine cases (60%) in patients over 5 years old. Seven cases (47%) were in males and eight cases (53%) were in females. Symptoms or clinical findings on hospital arrival included fever in 12 cases (80%), disturbance of consciousness in 10 (67%), nausea and/or vomiting in nine (60%), seizure in five (33%), inadequate intake of nutrition in five (33%), cough in four (27%), and no cases (0%) with dyspnea. In the medical institutions, the main diseases suspected of causing death were CNS abnormalities (n=5, 33%), cardiac abnormalities (n=4, 27%), other disease (n=3, 20%), unknown cause of death (n=3, 20%), and respiratory abnormalities (n=0, 0%). Date of onset was obtained in 14 of the 15 cases, and the number of days from onset to death was a median of 4.5 days (range: 0–15 days), with five patients (36%) dying in 0–2 days, four dying (29%) in 3–6 days, and five dying (36%) in 7 days or more.
Table. Characteristics of fatal cases under 20 years of age after SARS-CoV-2 infection (n=29; limited to clearly endogenous deaths occurring only from January 1 to August 31, 2022; as of August 31, 2022)
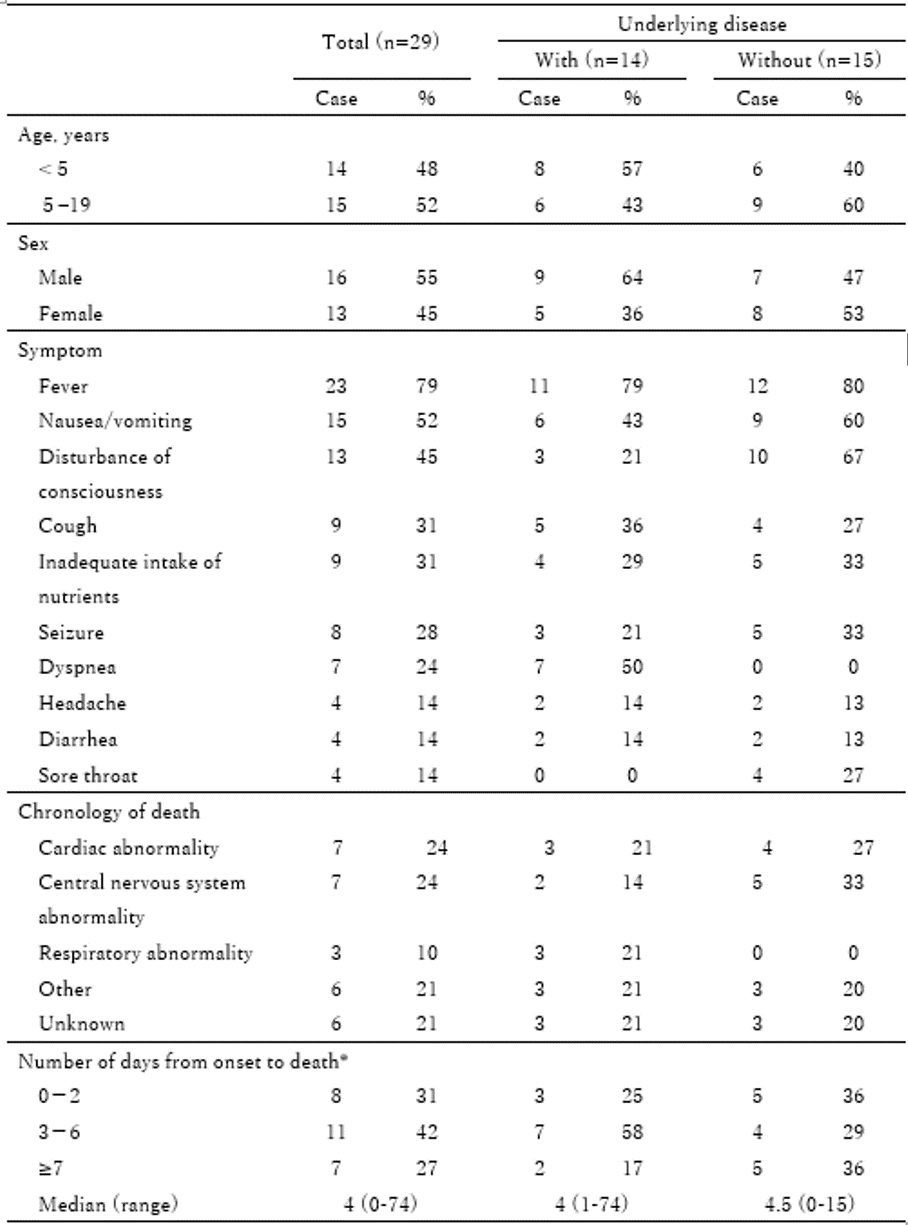
* Three cases whose date of onset or death was uncertain were excluded. Included were 12 cases with underlying disease and 14 cases without underlying disease.
Discussion
As of August 31, 2022, we described the interim report on 41 fatal pediatric cases from January 1 to August 31, 2022.
The number of cases had increased from mid-July 2022. In this field investigation, fatal pediatric cases caused by clearly endogenous factors included those in patients not only with underlying disease but also in patients with no underlying disease. Thus, families and healthcare workers might need to carefully follow the course of symptoms in those after SARS-CoV-2 infection. SARS-CoV-2 immunization was not administered in many of the fatal pediatric cases even though the children were of an approved age for the immunization. Moreover, compared to the registry of Japanese children with COVID-19 done by the Japan Pediatrics Society 2), the symptoms of the fatal pediatric cases in this investigation, except for respiratory symptoms, included a high proportion of nausea and/or vomiting (52%), disturbance of consciousness (45%), inadequate intake of nutrition (31%), and seizure (28%). The severity of COVID-19 is mainly classified only according to respiratory symptoms 3), but our results suggested that pediatric cases should be carefully followed up not only for respiratory symptoms but also for symptoms of CNS abnormalities such as disturbance of consciousness and seizure, vomiting, and inadequate intake of nutrients. The duration from onset to death was under one week in 73% of the patients, and our results further suggested that careful follow-up of the cases was important especially for the first week after onset of the disease.
Limitations and further investigation
This was an interim report as of August 31, 2022, and as the field investigation will continue to collect additional information on the fatal pediatric cases, the report may be revised and/or further information may be added, and we did not examine the causal relationship between SARS-CoV-2 infection and death. Therefore, the results should be carefully interpreted.We plan to continue to investigate fatal pediatric cases in cooperation with the local public health authorities and related academic associations.
Collaborating academic associations
Japan Pediatric Society, The Japanese Society of Intensive Care Medicine, Japanese Association for Acute Medicine.
References
1. Ministry of Health, Labour, and Welfare. Visualizing the data: information on COVID-19 infections. https://covid19.mhlw.go.jp/en/ (accessed on August 19, 2022).
2. Committee on Immunization and Prevention of Infectious Diseases, Japan Pediatric Society. Interim Report on Clinical Course of Domestic-Onset Pediatric Coronavirus Disease 2019 (COVID-19) Cases Using a Database: 3rd Report. Changes in Clinical Symptoms and Severity of Pediatric COVID-19 Cases Associated with the Omicron Epidemic. http://www.jpeds.or.jp/uploads/files/20220328_tyukan_hokoku3.pdf (accessed on August 19, 2022) [in Japanese].
3. Medical Treatment Guidance Review Committee. COVID-19 Treatment guidelines, the 8th Edition. https://www.mhlw.go.jp/content/000967699.pdf (accessed on August 19, 2022) [in Japanese].
- Details
102nd Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (October 12, 2022) Material 1
Evaluation of the latest infection status, etc.
Overview of the infection status
- The number of new cases of infection nationwide (by date of report) continued to decrease to approximately 143 per 100,000 in the last week, with a ratio to the previous week of 0.73.
However, attention must be paid to the impact of increased opportunities of contact due to consecutive holidays on the infection status. - With the decrease in the number of new cases of infection, the number of patients receiving treatment is also decreasing. The use rate of beds is also decreasing and improvement is seen in the situation of the medical care provision system.
The numbers of severe cases and deaths continue to show a downward trend.
Local trends
* The value for new cases of infection is the number of persons per 100,000 among the total number for the latest week, based on the reporting dates.
- Hokkaido
The number of new cases of infection was approximately 223 (approximately 216 in Sapporo City), and the ratio to the previous week is 0.80. The use rate of beds is approximately 20%.
- North Kanto
In Ibaraki, Tochigi, and Gunma, the numbers of new cases of infection were roughly 153, 130, and 162, respectively, and the ratios to the previous week were 0.67, 0.70 and 0.72, respectively.
The use rates of beds are slightly below 30% in Ibaraki, slightly below 20% in Tochigi, and slightly above 20% in Gunma. - Tokyo metropolitan area (Tokyo and 3 neighboring prefectures)
The number of new cases of infection in Tokyo was approximately 131, and the ratio to the previous week was 0.67. The use rate of beds is slightly over 10%, and the use rate of beds for severe cases is slightly below 10%.
In Saitama, Chiba, and Kanagawa, the numbers of new cases of infection were approximately 121, 116, and 128, respectively, and the ratios to the previous week were 0.69, 0.71, and 0.69, respectively.
The use rates of beds are slightly over 20% in Kanagawa, approximately 20% in Saitama and slightly over 10% in Chiba. - Chukyo/Tokai
The number of new cases of infection in Aichi was approximately 113, and the ratio to the previous week is 0.61. The use rate of beds is slightly over 20%.
In Gifu, Shizuoka, and Mie, the numbers of new cases of infection were about 150, 143, and 186, respectively, and the ratios to the previous week were 0.66, 0.78, and 0.78, respectively.
The use rates of beds are approximately 10% in Gifu, slightly over 10% in Shizuoka, and approximately 20% in Mie. - Kansai area
The number of new cases of infection in Osaka was approximately 143, and the ratio to the previous week was 0.69. The use rate of beds is slightly over 10%, while the use rate of beds for severe cases is below 10%.
In Shiga, Kyoto, Hyogo, Nara, and Wakayama, the numbers of new cases of infection were approximately 146, 110, 114, 134, and 167, respectively, and the ratios to the previous week were 0.64, 0.69, 0.73, 0.79, and 0.86, respectively.
The use rates of beds were slightly over 20% in Shiga, slightly over 10% in Hyogo, Kyoto and Nara, and approximately 10% in Wakayama. - Kyushu
The number of new cases of infection in Fukuoka was approximately 114, and the ratio to the previous week was 0.74. The use rate of beds is slightly over 10%.
In Saga, Nagasaki, Kumamoto, Oita, Miyazaki, and Kagoshima, the numbers of new cases of infection were approximately 123, 115, 130, 131, 135, and 129, respectively, and the ratios to the previous week were 0.57, 0.67, 0.74, 0.73, 0.75, and 0.70, respectively. The use rates of beds are slightly over 10% in Kumamoto, Oita, and Miyazaki, slightly below 20% in Nagasaki and Kagoshima, and approximately 10% in Saga. - Okinawa
The number of new cases of infection was approximately 142, and the ratio to the previous week was 0.70. The use rate of beds was slightly over 10%, while the use rate of beds for severe cases was approximately 10%.
- Areas other than the above
In Fukushima, Nagano, and Hiroshima, the ratios to the previous week were 0.91, 0.91 and 0.92, respectively. The use rate of beds was slightly below 10% in Fukui and Yamanashi.
Infection status and future outlook
Infection status
- The number of new cases of infection continues to decrease in all regions. However, outbreaks in facilities for elderly people and medical facilities have decreased despite continuing to some extent.
- The number of new cases of infection in each age group continues to decrease nationwide, but per population, the numbers are higher in younger age groups. The number of new cases of infection among elderly people has also been decreasing, and the numbers of severe cases and deaths also continue to show a downward trend.
- As the provisional report on the deaths of children since January this year suggests, attention must be paid to the occurrence of severe cases and deaths associated with an increase in the number of infected children.
Future outlook
- Regarding the future infection status, the number of infections may gradually decrease or remain at a constant level despite uncertainty, based on the short-term forecast in large cities. It is also necessary to pay attention to the impact that increased contact opportunities due to consecutive holidays and tourism will have on the infection status. In addition, based on the trends of the past two years, there are concerns about the spread of the new coronavirus infection this winter, an earlier seasonal flu epidemic than usual, and that these two may occur simultaneously.
Factors that increase and suppress infection
- [Immunization by vaccination and infection]
Immunity acquired from vaccination and natural infection may decline over time. Although the vaccination rate is higher among people in their 60s and older than those in their 20s to 40s, the acquisition of immunity by infection is lower, and there is concern about the spread of infection among elderly people in the future.
- [Contact patterns]
The nighttime population is decreasing in many areas due to a continued decline in temperature and rainfall. This may have contributed to the recent decrease in the number of infected people. However, there is also concern that the nighttime population will increase toward the end of the year.
- [Epidemic strain]
The BA.5 lineage has largely become mainstream and is replacing others. At present, there is no trend toward further replacement by other lineages.
- [Climatic factors]
Weather conditions will be favorable for ventilation for a while, but ventilation may be difficult on days with high temperatures or heavy rainfall.
Situation of the medical care provision system
- Nationwide, the use rate of beds is decreasing due to continued improvement of the infection situation, at a low level below 30% in all areas.
The use rate of beds for severe cases is also declining, and areas with a use rate of 0 are increasing. - Nationwide, the situation of the medical care provision system is improving, including general medical care. However, in the field of nursing care, patients are being treated in the facilities and infections are seen among workers.
Measures to be taken
Basic concepts
Regarding measures under the Infectious Disease Control Law, appropriate medical care will be provided to elderly people and persons at risk of severe illness, and the period of medical treatment of patients will be reviewed.
The spread of infections this summer and measures to handle the current infection situation will be reviewed, and measures will be taken based on the assumption that infections may spread due to a simultaneous epidemic of seasonal influenza this fall.
Each citizen will be asked to take voluntary actions to prevent infection, while strengthening and prioritization of the health care system will be promoted to protect those at high risk of becoming seriously ill, such as elderly people, and to ensure regular medical care.
The national and local governments will remind the public of the need for routine infection control measures and take measures to support the public's efforts to prevent infection.
- 1. Further promotion of vaccination
- As for the “vaccine for the Omicron variant," vaccination of all persons aged 12 and over who have completed the first vaccination should proceed.
- Vaccination for the BA.4 and BA.5 lineage has also started. As both vaccines for the BA.1 and for the BA.4 and BA.5 lineages are expected to be more effective than the previous vaccines, it is necessary to proceed with vaccination with vaccines that can be given earlier. The vaccination interval was set at 5 months, but it is necessary to consider shortening the vaccination interval in light of overseas trends, and to reach a conclusion by the end of October.
- Those who have not received vaccination will be encouraged to consider getting the initial vaccination as soon as possible.
- For children (ages 5 to 11), booster vaccinations will be promoted along with the initial vaccination.
- The initial vaccination for children (aged 6 months to 4 years) has been approved by the PMDA and positioned as an extraordinary vaccination, and initial vaccination in this age group will proceed.
- 2. Use of tests
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, the national and local governments are required to secure a system that enables testing, and further utilize testing.
- Perform frequent tests (about 2 or 3 times a week for facility workers) for workers at facilities for elderly people.
- Establishment of a self-testing system for fever outpatients should be further promoted, in which patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Promote further utilization of antigen qualitative test kits, such as by online sales through OTC.
- 3. Securing a medical care provision system
Prefectural governments must take measures to avoid overcrowding of beds and fever outpatient sections with the support of the national government.
- In addition to facilitating the use of available hospital beds and developing temporary medical facilities to supplement hospital beds, making efforts to avoid a shortage of hospital beds and emergency medical care, such as utilization of lodging facilities and resting beds
- Making appropriate adjustments so that patients requiring inpatient treatment can be hospitalized preferentially, performing frequent tests at facilities for elderly people, etc., and further strengthening medical support
- Securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule
- Promotion of effective and less burdensome measures against infection, such as flexible and efficient use of hospital beds through zoning of each hospital room
- Expansion and promotion of fever outpatient services, including the use of online medical care, etc., and further promotion of the development of a “fever outpatient self-examination system”
- Local residents should be informed that they should refrain from visiting an emergency outpatient unit only to receive a precautionary examination without symptoms, according to the actual situation in the region. In addition, in order to respond to concerns and questions at the time of worsening physical conditions, the consultation service by healthcare professionals via telephone should be thoroughly publicized, and this service should also be strengthened.
- Ensuring that workplaces and schools do not require test certificates at the start of medical treatment
- 4. Change of thinking about medical treatment and review of all-case notification
- Based on the review of the nationwide notification of all cases that began on September 26th, the health care system will be strengthened and prioritized to protect those who are at high risk of becoming seriously ill, and it is necessary to establish an environment where young people with mild symptoms, who are not subject to notification, can be assured of treatment at home.
- 5. Review of home care period
- Since the risk of infection remains in the shortened period of home care for those who test positive, they should monitor their own physical condition, such as measuring temperature, and take thorough measures against infection when going out. In addition, they must be asked to avoid contact with people who are at risk of becoming seriously ill, such as the elderly.
- To allow the minimum necessary outings, such as shopping for groceries, after 24 hours have passed since symptoms have subsided or when there are no symptoms, it is necessary to take voluntary actions to prevent infection, such as wearing a mask when going out or coming into contact with people, keeping contact with people to a short period of time, and not using public transportation.
- 6. Surveillance
- Deterioration of the accuracy of current surveillance is a concern due to the limited scope of notification, prioritization of notification items, delays in testing and diagnosis/reporting due to many infections, and changes in healthcare-seeking behavior. It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status.
It is also necessary to continue monitoring the trends of variants through genomic surveillance.
- Deterioration of the accuracy of current surveillance is a concern due to the limited scope of notification, prioritization of notification items, delays in testing and diagnosis/reporting due to many infections, and changes in healthcare-seeking behavior. It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status.
- 7. Effective ventilation
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, it is necessary to publicize and recommend effective ventilation methods to prevent insufficient indoor ventilation (how to create airflow considering aerosols, installation of partitions that do not block airflow, etc.).
- 8. Re-inspection and implementation of basic infection control
Re-inspection and implementation of the following basic infection control measures are needed.
- Continue proper wearing of nonwoven masks according to the situation, hand hygiene, thorough ventilation, etc.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, or loud voices.
- Eating and drinking should be done with as few people as possible, and masks should be worn except while eating and drinking.
- People with symptoms such as sore throat, cough, and fever should refrain from going out.
- Refer to guidelines for hospital visits and use of an ambulance.
- To reduce the chances of contact as far as possible, it is necessary for measures at the workplace, such as again promoting the use of telework.
- Organizers of events, meetings, and such should fully evaluate the epidemic situation and risk of infection in the area, and consider whether or not to hold the meeting, and if it is held, measures should be taken to minimize the infection risk.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is considered to have occurred via the same routes as before (droplets adhering to mucosa, aerosol inhalation, contact infection, etc.).
- [Severity]
It has been suggested that infection with the Omicron variant presents a lower risk of hospitalization or aggravation than the Delta variant. However, analyses to date show that the fatality due to infection with the Omicron variant is higher than that due to seasonal influenza. It is also suggested that the incidence of pneumonia is higher than that of seasonal influenza, but given the limited data, it needs to be investigated by various analyses. In the death toll from the previous outbreak compared to last summer's outbreak, it is reported that there are many cases in which the new coronavirus infection is not the direct cause of death, for example, people who have been in a facility for the elderly before the infection are infected and die due to the worsening of the underlying disease. In the current spread of infection, the rate of severe cases has continued to decrease and the ratio of elderly people among hospitalized patients has increased compared to the previous summer, following the previous outbreak. Among the deaths in this outbreak, mechanical ventilation/nasal high flow use rates and steroid prescription rates have decreased compared to the previous outbreak.
Among fatal cases in which endogenous death was identified in infected children, cases without underlying diseases were also found. Preliminary reports on the results of on-site investigations have stated that it is necessary to pay attention to neurological symptoms such as convulsions and disturbance of consciousness, and systemic symptoms other than respiratory symptoms such as vomiting and poor oral intake.
- [Virus shedding period]
According to Japanese data, risk of infection remains until 10 days after onset, and infectivity is high until 7 days after onset. Even after waiting for 5 days, 1/3 of patients are still shedding infectious viruses. On Day 8 (after waiting 7 days), most patients (approximately 85%) had not shed infectious virus, and it was reported that even in those who shed the virus, the amount of virus decreased to one-sixth after 7 days compared to the initial stage.
- [Vaccine effect]
For infection with the Omicron variant, the preventive effects of a first vaccination against infection and disease onset are markedly reduced. Its preventive effect on hospitalization is reported to be maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing effect, onset-preventing effect, and hospitalization-preventing effect against infection by the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Regarding the fourth vaccination, it has been reported that while the preventive effect against aggravation was not reduced for 6 weeks, the preventive effect against infection lasted only for a short time.
- [Sublineages of the Omicron variant]
Worldwide, the proportion of the BA.5 lineage is increasing while the number of positive cases increases, suggesting that this lineage is superior to the BA.2 lineage in terms of causing an increase in the number of infected people, but currently the number of positive cases is decreasing. The BA.5 lineage has shown a tendency to escape existing immunity compared with the BA.1 and BA.2 lineages, but no clear findings on the infectivity have been shown. The effective reproduction number of the BA.5 lineage calculated based on the data of Tokyo was about 1.27 times that of BA.2. It was also estimated that it was about 1.3 times higher in samples collected from private testing institutions nationwide.
According to the WHO report, the severity of BA.5 lineage shows both increased and unchanged data compared to the existing Omicron variants, and continued information collection is needed. In addition, the pathogenicity of the BA.5 lineage is reportedly higher than that of the BA.1 and BA.2 lineages, based on Japanese laboratory data, but it has not been confirmed clinically at this time. According to genomic surveillance in Japan, the detection rate of the BA.5 lineage has increased, and the previous dominant variant has largely been replaced with this lineage.
In addition, the BA.2.75 lineage, which has been reported mainly in India since June, and the BA.4.6 lineage reported mainly in the US and UK, have been detected in Japan. However, no clear findings have been obtained overseas regarding its infectivity or severity, compared with other lineages. It is necessary to continue to collect and analyze the situation and findings in other countries regarding these characteristics of the virus, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)
- Details
101st Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (October 5, 2022) Material 1
Evaluation of the latest infectious status, etc.
Overview of the infection status
- The number of new cases of infection nationwide (by date of report) continued to decrease to about 197 per 100,000 in the last week, with a ratio to the previous week of 0.65.
However, attention must be paid to the impact of increased opportunities of contact due to consecutive holidays on the infection status. - With the number of new cases of infection decreasing, the number of patients being treated is also decreasing. The use rate of beds is also decreasing; improvements can be seen in the situation of the medical care provision system.
Although the numbers of severe cases and deaths continue to decline, they are leveling off.
Local trends
* The value for new cases of infection is the number of persons per 100,000 among the total number for the latest week, based on the reporting dates.
- Hokkaido
The number of new cases of infection was approximately 279 (approximately 266 in Sapporo City), with a ratio to the previous week of 0.82. The use rate of beds is approximately 20%.
- North Kanto
In Ibaraki, Tochigi, and Gunma, the numbers of new cases of infection were roughly 228, 185, and 224, with ratios to the previous week of 0.88, 0.68 and 0.77, respectively.
The use rates of beds are approximately 40% in Ibaraki, and slightly more than 20% in Tochigi and Gunma. - Tokyo metropolitan area (Tokyo and 3 neighboring prefectures)
The number of new cases of infection in Tokyo was approximately 197, with a ratio to the previous week of 0.61. The use rate of beds is slightly less than 20%, while the use rate of beds for severe cases is approximately 10%.
In Saitama, Chiba, and Kanagawa, the numbers of new cases of infection were approximately 176, 163, and 184, with ratios to the previous week of 0.57, 0.54, and 0.73, respectively.
The use rates of beds are slightly more than 20% in Kanagawa and Saitama, and approximately 20% in Chiba. - Chukyo/Tokai
The number of new cases of infection in Aichi was approximately 186, with a ratio to the previous week of 0.58. The use rate of beds is slightly more than 20%.
In Gifu, Shizuoka, and Mie, the numbers of new cases of infection were about 226, 183, and 239, with ratios to the previous week of 0.78, 0.67, and 0.75, respectively.
The use rates of beds are slightly more than 10% in Gifu and Shizuoka, and approximately 20% in Mie. - Kansai area
The number of new cases of infection in Osaka was approximately 207, with a ratio to the previous week of 0.59. The use rate of beds is approximately 20%, while the use rate of beds for severe cases is less than 10%.
In Shiga, Kyoto, Hyogo, Nara, and Wakayama, the numbers of new cases of infection were about 229, 158, 156, 170, and 195, with ratios to the previous week of 0.61, 0.57, 0.59, 0.51, and 0.64, respectively.
The use rates of beds are slightly more than 20% in Shiga, slightly less than 20% in Hyogo and Nara, and slightly more than 10% in Kyoto and Wakayama. - Kyushu
The number of new cases of infection in Fukuoka was approximately 156, with a ratio to the previous week of 0.61. The use rate of beds is slightly less than 20%.
In Saga, Nagasaki, Kumamoto, Oita, Miyazaki, and Kagoshima, the numbers of new cases of infection were about 218, 171, 176, 180, 180, and 184, with ratios to the previous week of 0.72, 0.62, 0.48, 0.63, 0.47, and 0.64, respectively. The use rates of beds are slightly less than 20% in Miyazaki, approximately 20% in Kumamoto and Kagoshima, and slightly more than 10% in Saga, Nagasaki, and Oita. - Okinawa
The number of new cases of infection was approximately 203, with a ratio to the previous week of 0.78. The use rate of beds is slightly less than 20%, while the use rate of beds for severe cases is slightly more than 10%.
- Areas other than the above
Miyagi, Toyama, Nagano, and Ehime had ratios to the previous week of 0.86, 0.87, 0.89, and 0.53, respectively. The use rate of beds is slightly less than 10% in Yamanashi.
Infection status and future outlook
Infection status
- The number of new cases of infection continues to decrease in all regions. In the Tohoku, Hokuriku-Koshinetsu, Chugoku, and Shikoku regions, infection levels were almost the same as the peak in February this year. On the other hand, there are regional differences, such as the rate of decrease slowing down in some regions, and a ratio to the previous week close to 1. Outbreaks in facilities for elderly people and medical facilities are decreasing, although they partially continue.
- The number of new cases of infection in each age group continues to decrease nationwide, but per population, the numbers are higher in younger age groups. The number of new cases of infection among the elderly has also been decreasing, and the numbers of severe cases and deaths continue to decrease but are leveling off.
- As the provisional report on the deaths of children since January this year suggests, attention must be paid to the occurrence of severe cases and deaths associated with the increase in the number of infected children.
Future outlook
- Regarding future infection status, although there are regional differences and uncertainties, the decreasing trend may continue in many regions, but the rate of decrease may slow in some regions, based on the epi curve of the date of onset and short-term forecast in large cities. It is also necessary to pay attention to the impact that increased contact opportunities due to consecutive holidays and tourism will have on the infection status. In addition, from the trends of the past two years, there are concerns about the spread of the new coronavirus infection this winter, the seasonal flu epidemic coming earlier than usual, and that these may occur simultaneously.
Factors that increase and suppress infection
- [Immunization by vaccination and infection]
Immunity acquired from vaccination and natural infection may decline over time. Although the vaccination rate is higher among people in their 60s and older than those in their 20s to 40s, the acquisition of immunity by infection is lower, and there is concern about the spread of infection among elderly people in the future.
- [Contact patterns]
Regarding the nighttime population, while the infection situation is improving in all regions, an increase is currently being seen in large cities such as Tokyo, Aichi, Osaka, and Fukuoka, as well as many regions such as Okinawa. There is also a concern that the nighttime population will further increase toward the end of the year.
- [Epidemic strain]
The BA.5 lineage has largely become mainstream and is replacing others. At present, there is no trend toward further replacement by other lineages.
- [Climatic factors]
Weather conditions will be favorable for ventilation for a while, but ventilation may be difficult on days with high temperatures or heavy rainfall.
Status of the medical care provision system
- Nationwide, the use rate of beds is decreasing due to the continued improvement of the infection situation, being at a low level of less than 30% in almost all areas. The use rate of beds for sever cases is also declining, and in some regions is zero.
- Nationwide, although there is some burden on the medical care provision system including general medical care, the situation is improving. In the field of nursing care, patients are being treated in the facilities and infections are seen among workers.
- Regarding cases of difficulty in emergency transport, the trend of improvement continues nationwide, especially in cases of suspected COVID-19.
Measures to be taken
Basic concepts
- Regarding measures under the Infectious Disease Control Law, appropriate medical care will be provided to the elderly and persons at risk of severe illness, and the period of medical treatment of patients will be reviewed.
- During this transition, the spread of infections this summer will be reviewed, along with measures to deal with the current infection situation, and measures will be taken based on the assumption that infections may spread due to simultaneous epidemic of seasonal influenza this fall.
- Each citizen will be asked to take voluntary actions to prevent infection, and the strengthening and prioritization of the health care system will be promoted in order to protect those at high risk of becoming seriously ill, such as the elderly, and to ensure regular medical care.
- The national and local governments will remind the public of the need for routine infection control measures, and take measures to support the public's efforts to prevent infection.
- 1. Further promotion of vaccination
- Preparations must proceed by mid-October for vaccination with the "vaccine for the Omicron variant" for all persons aged 12 and over who have completed the first vaccination.
- By mid-October, the vaccine used the 4th vaccination, which is administered for reasons such as a high risk of severe illness, will be switched from the conventional vaccine to the vaccine for the Omicron variant. The vaccination interval was set at 5 months, but it is necessary to consider shortening the vaccination interval in light of overseas trends, and to reach a conclusion by the end of October.
- Those who have not received vaccination will be encouraged to consider getting the initial vaccination as soon as possible.
- For children (ages 5 to 11), booster vaccinations will be promoted along with the initial vaccination.
- 2. Use of tests
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, the national and local governments are required to secure a system that enables testing, and further utilize testing.
- Perform frequent tests (about 2 or 3 times a week for facility workers) for workers at facilities for elderly people.
- Establishment of a self-testing system for fever outpatients should be further promoted, in which patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Promote further utilization of antigen qualitative test kits, such as by online sales through OTC.
- 3. Securing a medical care provision system
- Prefectural governments must take measures to avoid overcrowding of beds and fever outpatient sections with the support of the national government.
- In addition to facilitating the use of available hospital beds and developing temporary medical facilities to supplement hospital beds, making efforts to avoid a shortage of hospital beds and emergency medical care, such as utilization of lodging facilities and resting beds
- Making appropriate adjustments so that patients requiring inpatient treatment can be hospitalized preferentially, performing frequent tests at facilities for elderly people, etc., and further strengthening medical support
- Securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule
- Promotion of effective and less burdensome measures against infection, such as flexible and efficient use of hospital beds through zoning of each hospital room
- Expansion and promotion of fever outpatient services, including the use of online medical care, etc., and further promotion of the development of a “fever outpatient self-examination system”
- Local residents should be informed that they should refrain from visiting an emergency outpatient unit only to receive a precautionary examination without symptoms, according to the actual situation in the region. In addition, in order to respond to concerns and questions at the time of worsening physical conditions, the consultation service by healthcare professionals via telephone should be thoroughly publicized, and this service should also be strengthened.
- Ensuring that workplaces and schools do not require test certificates at the start of medical treatment
- 4. Change of thinking about medical treatment and review of all-case notification
- Based on the review of the nationwide notification of all cases that began September 26th, the health care system will be strengthened and prioritized to protect those who are at high risk of becoming seriously ill, and it is necessary to establish an environment where young people with mild symptoms who are not subject to notification can be assured of treatment at home.
- 5. Review of home care period
- Since the risk of infection remains in the shortened period of home care for those who test positive, they should monitor their own physical condition, such as measuring temperature, and take thorough measures against infection when going out. In addition, they must be asked to avoid contact with people who are at risk of becoming seriously ill, such as the elderly.
- To allow the minimum necessary outings, such as shopping for groceries, after 24 hours have passed since symptoms have subsided or when there are no symptoms, it is necessary to take voluntary actions to prevent infection, such as wearing a mask when going out or coming into contact with people, keeping contact with people to a short period of time, and not using public transportation.
- 6. Surveillance
- Deterioration of the accuracy of current surveillance is a concern due to the limited scope of notification, prioritization of notification items, delays in testing and diagnosis/reporting due to many infections, and changes in healthcare-seeking behavior. It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status.
It is also necessary to continue monitoring the trends of variants through genomic surveillance.
- Deterioration of the accuracy of current surveillance is a concern due to the limited scope of notification, prioritization of notification items, delays in testing and diagnosis/reporting due to many infections, and changes in healthcare-seeking behavior. It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status.
- 7. Effective ventilation
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, it is necessary to publicize and recommend effective ventilation methods to prevent insufficient indoor ventilation (how to create airflow considering aerosols, installation of partitions that do not block airflow, etc.).
- 8. Re-inspection and implementation of basic infection control
Re-inspection and implementation of the following basic infection control measures are needed.
- Continue proper wearing of nonwoven masks according to the situation, hand hygiene, thorough ventilation, etc.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, or loud voices.
- Eating and drinking should be done with as few people as possible, and masks should be worn except while eating and drinking.
- People with symptoms such as sore throat, cough, and fever should refrain from going out.
- Refer to guidelines for hospital visits and use of an ambulance.
- To reduce the chances of contact as far as possible, measures at the workplace are needed, such as again promoting the use of telework.
- Organizers of events, meetings, and such should fully evaluate the epidemic situation and risk of infection in the area, and consider whether or not to hold the meeting, and if it is held, measures should be taken to minimize the infection risk.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is considered to have occurred via the same routes as before (droplets adhering to mucosa, aerosol inhalation, contact infection, etc.).
- [Severity]
It has been suggested that infection with the Omicron variant presents a lower risk of hospitalization or aggravation than the Delta variant. However, analyses to date show that the fatality due to infection with the Omicron variant is higher than that due to seasonal influenza. It is also suggested that the incidence of pneumonia is higher than that of seasonal influenza, but given the limited data, it needs to be investigated by various analyses. In the death toll from the previous outbreak compared to last summer's outbreak, it is reported that there are many cases in which the new coronavirus infection is not the direct cause of death, for example, people who have been in a facility for the elderly before the infection are infected and die due to the worsening of the underlying disease. In the current spread of infection, the rate of severe cases has continued to decrease and the ratio of elderly people among hospitalized patients has increased compared to the previous summer, following the previous outbreak. Among the deaths in this outbreak, mechanical ventilation/nasal high flow use rates and steroid prescription rates have decreased compared to the previous outbreak.
Among fatal cases in which endogenous death was identified in infected children, cases without underlying diseases were also found. Preliminary reports on the results of on-site investigations have stated that it is necessary to pay attention to neurological symptoms such as convulsions and disturbance of consciousness, and systemic symptoms other than respiratory symptoms such as vomiting and poor oral intake.
- [Virus shedding period]
According to Japanese data, risk of infection remains until 10 days after onset, and infectivity is high until 7 days after onset. Even after waiting for 5 days, 1/3 of patients are still shedding infectious viruses. On Day 8 (after waiting 7 days), most patients (approximately 85%) had not shed infectious virus, and it was reported that even in those who shed the virus, the amount of virus decreased to one-sixth after 7 days compared to the initial stage.
- [Vaccine effect]
For infection with the Omicron variant, the preventive effects of a first vaccination against infection and disease onset are markedly reduced. Its preventive effect on hospitalization is reported to be maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing effect, onset-preventing effect, and hospitalization-preventing effect against infection by the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Regarding the fourth vaccination, it has been reported that while the preventive effect against aggravation was not reduced for 6 weeks, the preventive effect against infection lasted only for a short time.
- [Sublineages of the Omicron variant]
Worldwide, the proportion of the BA.5 lineage is increasing while the number of positive cases increases, suggesting that this lineage is superior to the BA.2 lineage in terms of causing an increase in the number of infected people, but currently the number of positive cases is decreasing. The BA.5 lineage has shown a tendency to escape existing immunity compared with the BA.1 and BA.2 lineages, but no clear findings on the infectivity have been shown. The effective reproduction number of the BA.5 lineage calculated based on the data of Tokyo was about 1.27 times that of BA.2. It was also estimated that it was about 1.3 times higher in samples collected from private testing institutions nationwide.
According to the WHO report, the severity of BA.5 lineage shows both increased and unchanged data compared to the existing Omicron variants, and continued information collection is needed. In addition, the pathogenicity of the BA.5 lineage is reportedly higher than that of the BA.1 and BA.2 lineages, based on Japanese laboratory data, but it has not been confirmed clinically at this time. According to genomic surveillance in Japan, the detection rate of the BA.5 lineage has increased, and the previous dominant variant has largely been replaced with this lineage.
In addition, the BA.2.75 lineage, which has been reported mainly in India since June, and the BA.4.6 lineage reported mainly in the US and UK, have been detected in Japan. However, no clear findings have been obtained overseas regarding its infectivity or severity, compared with other lineages. It is necessary to continue to collect and analyze the situation and findings in other countries regarding these characteristics of the virus, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)
- Details
100th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (September 21, 2022) Material 1
Evaluation of the latest infectious status, etc.
Overview of the infection status
- The number of new cases of infection nationwide (by date of report) continued to decrease to about 370 per 100,000 in the last week, with the ratio to the previous week at 0.71.
Nationwide, the infection level was below the peak in February this year. However, attention should be paid to the impact of consecutive holidays on the infection status. - With the number of new cases of infection decreasing, the number of patients being treated is also decreasing. The use rate of beds is also declining.
Although the burden on the medical care provision system partially continues, the situation is improving.
The numbers of severe cases and deaths continue to decrease.
Local trends
* The value for new cases of infection is the number of persons per 100,000 among the total number for the latest week, based on the reporting dates.
- Hokkaido
The number of new cases of infection was approximately 344 (approximately 386 in Sapporo City), with a ratio to the previous week of 0.68. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly less than 30%.
- North Kanto
In Ibaraki, Tochigi, and Gunma, the numbers of new cases of infection were roughly 353, 296, and 354, with ratios to the previous week of 0.82, 0.70 and 0.77, respectively.
The use rates of beds are slightly more than 40% in Ibaraki, slightly more than 20% in Tochigi, and approximately 30% in Gunma. - Tokyo metropolitan area (Tokyo and 3 neighboring prefectures)
The number of new cases of infection in Tokyo was approximately 370, with a ratio to the previous week of 0.79. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly less than 30%, while the use rate of beds for severe cases is slightly more than 20%.
In Saitama, Chiba, and Kanagawa, the numbers of new cases of infection were approximately 407, 349, and 315, with ratios to the previous week of 0.87, 0.80, and 0.82, respectively. The use rates of beds are slightly more than 30% in Saitama, about 30% in Chiba and about 40% in Kanagawa. - Chukyo/Tokai
The number of new cases of infection in Aichi was approximately 408, with a ratio to the previous week of 0.68. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 50%.
In Gifu, Shizuoka, and Mie, the numbers of new cases of infection were about 360, 368, and 515, with ratios to the previous week of 0.58, 0.67, and 0.94, respectively. The use rates of beds are slightly more than 30% in Gifu, approximately 30% in Shizuoka, and slightly less than 40% in Mie. - Kansai area
The number of new cases of infection in Osaka was approximately 390, with a ratio to the previous week of 0.68. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 30%, while the use rate of beds for severe cases is less than 10%.
In Shiga, Kyoto, Hyogo, Nara, and Wakayama, the numbers of new cases of infection were about 452, 409, 373, 417, and 364, with ratios to the previous week of 0.70, 0.72, 0.67, 0.72, and 0.66, respectively. The use rates of beds are slightly less than 40% in Shiga, slightly more than 30% in Hyogo and Wakayama, slightly less than 30% in Kyoto, and slightly more than 20% in Nara. - Kyushu
The number of new cases of infection in Fukuoka was approximately 331, with a ratio to the previous week of 0.62. The infected individuals are mainly in their 30s or younger. The use rate of beds is approximately 30%.
In Saga, Nagasaki, Kumamoto, Oita, Miyazaki, and Kagoshima, the numbers of new cases of infection were about 342, 298, 369, 329, 451, and 498, with ratios to the previous week of 0.56, 0.49, 0.61, 0.57, 0.59, and 0.62, respectively. The use rates of beds are slightly less than 40% in Oita, Kumamoto, and Nagasaki, slightly more than 30% in Kagoshima, and slightly more than 20% in Miyazaki and Saga. - Okinawa
The number of new cases of infection was approximately 277, with a ratio to the previous week of 0.60. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 30%, while the use rate of beds for severe cases is about 20%.
- Areas other than the above
In Hiroshima and Kagawa, the ratios to the previous week were 0.80 and 0.81, respectively. The use rates of beds are about 40% in Kagawa, slightly less than 20% in Kochi, and slightly more than 10% in Yamanashi.
Infection status and future outlook
Infection status
- The number of new cases of infection continued to decrease in all regions, and nationwide the infection level was below the peak in February this year. However, the rate of decrease has slowed down in Tokyo and other metropolitan areas, and in areas where the February peak was relatively low, such as Tohoku, Hokuriku, Chugoku, and Shikoku, the infection level still exceeds that peak. Outbreaks in facilities for elderly people and medical facilities continue, although they are decreasing.
- The number of new cases of infection in each age group continues to decrease nationwide, but the number of patients under the age of 10 is larger than other age groups. In some regions, such as Tokyo and Saitama, the number of those in their teens increased. The number of new cases of infection among the elderly has also been decreasing, and the numbers of severe cases and deaths continue to decrease.
- As the provisional report on the deaths of children since January this year suggests, attention must be paid to the occurrence of severe cases and deaths associated with the increase in the number of infected children.
- Regarding the places of infection of newly infected people, due to the reopening of schools, an increasing trend continues in schools, etc., but it is currently decreasing. (Due to the emphasis on active epidemiological surveys, the route of infection is only understood in some cases [about 13%], and the effect of consecutive holidays should be noted.)
Future outlook
- Regarding future infection status, although there are regional differences and uncertainties, the decreasing trend may continue in many regions, but the rate of decrease may slow in some regions, based on the epi curve of the date of onset and short-term forecast in large cities. Attention should be paid to the impact of consecutive holidays on the infection status. In addition, there are concerns that the seasonal flu epidemic may be earlier than usual, and that new coronavirus infections may occur simultaneously.
Factors that increase and suppress infection
- [Vaccination and immunity from infection]
It has become clear that as a certain period elapses after the third vaccination, the infection prevention effect is attenuated compared to the aggravation prevention effect. On the other hand, those in their 60s and older are less likely to acquire immunity by infection than those in their 20s to 40s. It is also pointed out that immunity is attenuated, and there is concern about the spread of infection among elderly people in the future.
- [Contact patterns]
Regarding the nighttime population, the tendency has been flat overall, despite increases in relatively many regions, and while the infection situation is improving in all regions, movements are uneven, with effects of the weather. Due to the effects of bad weather such as rain and typhoons, it is necessary to pay attention to the increase in contact opportunities with the three Cs indoors rather than outdoors.
- [Epidemic strain]
The BA.5 lineage has largely become mainstream and is replacing others. At present, there is no trend toward further replacement by other lineages.
- [Climatic factors]
In the future, ventilation may be difficult on days with high temperatures or heavy rainfall.
Status of the medical care provision system
- Nationwide, the burden on the outpatient examination system is evident, and the use rate of beds is decreasing due to the continued improvement of the infection situation, being under 50% in almost all areas. The use rate of beds for sever cases is also declining. In addition, the numbers of home care recipients and medical treatment adjustments are on a decreasing trend in all areas where the data is available.
- Nationwide, although the burden on the medical care provision system including general medical care partially continues, the situation is improving. In the field of nursing care, patients are being treated in facilities and infection among workers continues.
Measures to be taken
Basic concepts
- Regarding measures under the Infectious Disease Control Law, appropriate medical care will be provided to the elderly and persons at risk of severe illness, and the period of medical treatment of patients will be reviewed.
- During this transition, the spread of infections this summer will be reviewed, along with measures to deal with the current infection situation, and measures will be taken based on the assumption that infections may spread due to simultaneous epidemic of seasonal influenza this fall.
- Each citizen will be asked to take voluntary actions to prevent infection, and the strengthening and prioritization of the health care system will be promoted in order to protect those at high risk of becoming seriously ill, such as the elderly, and to ensure regular medical care.
- The national and local governments will remind the public of the need for routine infection control measures and take measures to support the public's efforts to prevent infection.
- 1. Further promotion of vaccinations
- Preparations must proceed by mid-October for vaccination with the "vaccine for the Omicron variant" for all persons aged 12 and over who have completed the first vaccination.
- By mid-October, the vaccine used the 4th vaccination, which is administered for reasons such as a high risk of severe illness, will be switched from the conventional vaccine to the vaccine for the Omicron variant. The vaccination interval was set at 5 months, but it is necessary to consider shortening the vaccination interval in light of overseas trends, and to reach a conclusion by the end of October.
- Those who have not received vaccination will be encouraged to consider getting the initial vaccination as soon as possible.
- For children (ages 5 to 11), booster vaccinations will be promoted along with the initial vaccination.
- 2. Use of tests
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, the national and local governments are required to secure a system that enables testing, and further utilize testing.
- Perform frequent tests (about 2 or 3 times a week for facility workers) for workers at facilities for elderly people.
- Establishment of a self-testing system for fever outpatients should be further promoted, in which patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Promote further utilization of antigen qualitative test kits, such as by online sales through OTC.
- 3. Securing a medical care provision system
- Prefectural governments must take measures to avoid overcrowding of beds and fever outpatient sections with the support of the national government.
- In addition to facilitating the use of available hospital beds and developing temporary medical facilities to supplement hospital beds, making efforts to avoid a shortage of hospital beds and emergency medical care, such as utilization of lodging facilities and resting beds
- Making appropriate adjustments so that patients requiring inpatient treatment can be hospitalized preferentially, performing frequent tests at facilities for elderly people, etc., and further strengthening medical support
- Securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule
- Promotion of effective and less burdensome measures against infection, such as flexible and efficient use of hospital beds through zoning of each hospital room
- Expansion and promotion of fever outpatient services, including the use of online medical care, etc., and further promotion of the development of a “fever outpatient self-examination system”
- Local residents should be informed that they should refrain from visiting an emergency outpatient unit only to receive a precautionary examination without symptoms, according to the actual situation in the region. In addition, in order to respond to concerns and questions at the time of worsening physical conditions, the consultation service by healthcare professionals via telephone should be thoroughly publicized, and this service should also be strengthened.
- Ensuring that workplaces and schools do not require test certificates at the start of medical treatment
- 4. Change of thinking about medical treatment and review of all-case notification
- In the review of the nationwide notification of all cases that begins on the 26th, the health care system will be strengthened and prioritized to protect those who are at high risk of becoming seriously ill, and it is necessary to establish an environment where young people with mild symptoms who are not subject to notification can be assured of treatment at home.
- 5. Review of home care period
- Since the risk of infection remains in the shortened period of home care for those who test positive, they should monitor their own physical condition, such as measuring temperature, and take thorough measures against infection when going out. In addition, they must be asked to avoid contact with people who are at risk of becoming seriously ill, such as the elderly.
- To allow the minimum necessary outings, such as shopping for groceries, after 24 hours have passed since symptoms have subsided or when there are no symptoms, it is necessary to take voluntary actions to prevent infection, such as wearing a mask when going out or coming into contact with people, keeping contact with people to a short period of time, and not using public transportation.
- 6. Surveillance
- Deterioration of the accuracy of current surveillance is a concern due to the limited scope of notification, prioritization of notification items, delays in testing and diagnosis/reporting due to many infections, and changes in healthcare-seeking behavior. It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status.
It is also necessary to continue monitoring the trends of variants through genomic surveillance.
- Deterioration of the accuracy of current surveillance is a concern due to the limited scope of notification, prioritization of notification items, delays in testing and diagnosis/reporting due to many infections, and changes in healthcare-seeking behavior. It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status.
- 7. Effective ventilation
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, it is necessary to publicize and recommend effective ventilation methods to prevent insufficient ventilation due to the use of air conditioners (how to create airflow considering aerosols, installation of partitions that do not block airflow, etc.).
- 8. Re-inspection and implementation of basic infection control
Re-inspection and implementation of the following basic infection control measures are needed.
- Continue proper wearing of nonwoven masks, hand hygiene, thorough ventilation, etc.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, or loud voices.
- Eating and drinking should be done with as few people as possible, and masks should be worn except while eating and drinking.
- People with symptoms such as sore throat, cough, and fever should refrain from going out.
- Refer to guidelines for hospital visits and use of an ambulance.
- To reduce the chances of contact as far as possible, it is necessary for measures at the workplace, such as again promoting the use of telework.
- Organizers of events, meetings, and such should fully evaluate the epidemic situation and risk of infection in the area, and consider whether or not to hold the meeting, and if it is held, measures should be taken to minimize the infection risk.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is considered to have occurred via the same routes as before (droplets adhering to mucosa, aerosol inhalation, contact infection, etc.).
- [Severity]
It has been suggested that infection with the Omicron variant presents a lower risk of hospitalization or aggravation than the Delta variant. However, analyses to date show that the fatality due to infection with the Omicron variant is higher than that due to seasonal influenza. It is also suggested that the incidence of pneumonia is higher than that of seasonal influenza, but given the limited data, it needs to be investigated by various analyses. In the death toll from the previous outbreak compared to last summer's outbreak, it is reported that there are many cases in which the new coronavirus infection is not the direct cause of death, for example, people who have been in a facility for the elderly before the infection are infected and die due to the worsening of the underlying disease. In the current spread of infection, the rate of severe cases has continued to decrease and the ratio of elderly people among hospitalized patients has increased compared to the previous summer, following the previous outbreak. Among the deaths in this outbreak, mechanical ventilation/nasal high flow use rates and steroid prescription rates have decreased compared to the previous outbreak.
Among fatal cases in which endogenous death was identified in infected children, cases without underlying diseases were also found. Preliminary reports on the results of on-site investigations have stated that it is necessary to pay attention to neurological symptoms such as convulsions and disturbance of consciousness, and systemic symptoms other than respiratory symptoms such as vomiting and poor oral intake.
- [Virus shedding period]
According to Japanese data, risk of infection remains until 10 days after onset, and infectivity is high until 7 days after onset. Even after waiting for 5 days, 1/3 of patients are still shedding infectious viruses. On Day 8 (after waiting 7 days), most patients (approximately 85%) had not shed infectious virus, and it was reported that even in those who shed the virus, the amount of virus decreased to one-sixth after 7 days compared to the initial stage.
- [Vaccine effect]
For infection with the Omicron variant, the preventive effects of a first vaccination against infection and disease onset are markedly reduced. Its preventive effect on hospitalization is reported to be maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing effect, onset-preventing effect, and hospitalization-preventing effect against infection by the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Regarding the fourth vaccination, it has been reported that while the preventive effect against aggravation was not reduced for 6 weeks, the preventive effect against infection lasted only for a short time.
- [Sublineages of the Omicron variant]
Worldwide, the proportion of the BA.5 lineage is increasing while the number of positive cases increases, suggesting that this lineage is superior to the BA.2 lineage in terms of causing an increase in the number of infected people, but currently the number of positive cases is decreasing. The BA.5 lineage has shown a tendency to escape existing immunity compared with the BA.1 and BA.2 lineages, but no clear findings on the infectivity have been shown. The effective reproduction number of the BA.5 lineage calculated based on the data of Tokyo was about 1.27 times that of BA.2. It was also estimated that it was about 1.3 times higher in samples collected from private testing institutions nationwide.
According to the WHO report, the severity of BA.5 lineage shows both increased and unchanged data compared to the existing Omicron variants, and continued information collection is needed. In addition, the pathogenicity of the BA.5 lineage is reportedly higher than that of the BA.1 and BA.2 lineages, based on Japanese laboratory data, but it has not been confirmed clinically at this time. According to genomic surveillance in Japan, the detection rate of the BA.5 lineage has increased, and the previous dominant variant has largely been replaced with this lineage.
In addition, the BA.2.75 lineage, which has been reported mainly in India since June, and the BA.4.6 lineage reported mainly in the US and UK, have been detected in Japan. However, no clear findings have been obtained overseas regarding its infectivity or severity, compared with other lineages. It is necessary to continue to collect and analyze the situation and findings in other countries regarding these characteristics of the virus, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)
- Details
99th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (September 14, 2022) Material 1
Evaluation of the latest infectious status, etc.
Overview of the infection status
- The number of new cases of infection nationwide (by date of report) was about 520 per 100,000 in the last week, and the ratio to the previous week continued to decrease at 0.76, and nationwide the infection level was almost the same as the peak in February this year. However, in some areas, the decrease in the number of infected people has slowed down, and it is necessary to continue to pay attention to the impact of the reopening of schools after the summer vacation and the upcoming consecutive holidays on the infection situation.
- With the number of new cases of infection decreasing, the number of patients being treated is also decreasing. The use rate of beds is also declining.
Although the burden on the medical care provision system is partly continuing, not only by COVID-19 but also general medical care, the situation has been improved.
The number of severe cases continues to decrease, and the number of deaths has also started to decrease.Effective reproduction number: On a national basis, the most recent number is 0.89 (as of August 28), while the figure stands at 0.91 in the Tokyo metropolitan area and 0.89 in the Kansai area.
Local trends
* The value for new cases of infection is the number of persons per 100,000 among the total number for the latest week, based on the reporting dates.
- Hokkaido
The number of new cases of infection was approximately 508 (approximately 520 in Sapporo City), with a ratio to the previous week of 0.79. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 30%.
- North Kanto
In Ibaraki, Tochigi, and Gunma, the numbers of new cases of infection were roughly 430, 422, and 459, with ratios to the previous week of 0.77, 0.81 and 0.80, respectively. In Tochigi and Gunma, they were mainly in their 30s or younger. The use rates of beds are slightly more than 40% in Ibaraki, and slightly more than 30% in Tochigi and Gunma.
- Tokyo metropolitan area (Tokyo and 3 neighboring prefectures)
The number of new cases of infection in Tokyo was approximately 468, with a ratio to the previous week of 0.81. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 30%, while the use rate of beds for severe cases is slightly more than 20%. In Saitama, Chiba, and Kanagawa, the numbers of new cases of infection were approximately 466, 434, and 384, with ratios to the previous week of 0.84, 0.80, and 0.87, respectively. The use rates of beds are slightly more than 40% in Saitama and Kanagawa and slightly more than 30% in Chiba.
- Chukyo/Tokai
The number of new cases of infection in Aichi was approximately 600, with a ratio to the previous week of 0.75. The infected individuals are mainly in their 30s or younger. The use rate of beds is approximately 70%. In Gifu, Shizuoka, and Mie, the numbers of new cases of infection were about 622, 548, and 548, with ratios to the previous week of 0.78, 0.83, and 0.67, respectively. The use rates of beds are approximately 40% in Shizuoka and slightly more than 40% in Gifu and Mie.
- Kansai area
The number of new cases of infection in Osaka was approximately 573, with a ratio to the previous week of 0.76. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 40%, while the use rate of beds for severe cases is about 10%. In Shiga, Kyoto, Hyogo, Nara, and Wakayama, the numbers of new cases of infection were about 647, 569, 558, 579, and 548, with ratios to the previous week of 0.83, 0.74, 0.74, 0.83, and 0.78, respectively. The use rates of beds are slightly more than 50% in Shiga, slightly more than 40% in Hyogo, Kyoto and Wakayama, and slightly more than 20% in Nara.
- Kyushu
The number of new cases of infection in Fukuoka was approximately 536, with a ratio to the previous week of 0.69. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 40%. In Saga, Nagasaki, Kumamoto, Oita, Miyazaki, and Kagoshima, the numbers of new cases of infection were about 615, 609, 602, 573, 768, and 807, with ratios to the previous week of 0.75, 0.63, 0.74, 0.73, 0.79, and 0.78, respectively. The use rates of beds are slightly more than 50% in Oita, slightly more than 40% in Nagasaki and Kagoshima, slightly less than 40% in Miyazaki, and slightly more than 30% in Saga and Kumamoto.
- Okinawa
The number of new cases of infection was approximately 462, with a ratio to the previous week of 0.56. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 40%, while the use rate of beds for severe cases is slightly more than 30%.
- Areas other than the above
Fukushima, Toyama, Fukui, and Shimane had ratios to the previous week of 0.80, 0.81, 0.85, and 0.81, respectively. The use rates of beds are slightly more than 40% in Aomori, Akita, Yamagata, Toyama, Ishikawa, Nagano, Okayama, Tokushima, and Kagawa.
Infection status and future outlook
Infection status
- The number of new cases of infection continued to decrease in all regions, and nationwide the infection level was almost the same as the peak in February this year. Outbreaks in facilities for elderly people and medical facilities continue, although they are decreasing.
- The number of new cases of infection in each age group continues to decrease nationwide, but the number of patients under the age of 10 is larger than other age groups. The number of new cases of infection among the elderly has also been decreasing, the number of severe cases continues to decrease, and the number of deaths has started to decrease.
- A provisional report was made on the deaths of children since January this year. Attention must be paid to the occurrence of severe cases and deaths associated with the increase in the number of infected children.
- Regarding the place of contracting new infections, the rate of infections that develop at home has tended to be flat for all ages, but it is increasing especially for those in their 20s. Due to the reopening of schools, the number of infections continues to increase at schools. (It should be noted that due to the emphasis on active epidemiological surveys, the route of infection is only understood in some cases [~13%].)
Future outlook and factors that increase and suppress infection
- Regarding future infection status, although there are regional differences and uncertainties, the decreasing trend may continue in many regions, but the rate of decrease may slow in some regions, based on the epi curve of the date of onset and short-term forecast in large cities. It is necessary to pay attention to the impact of the resumption of school after the summer vacation and the upcoming consecutive holidays. In addition, there are concerns that the seasonal flu epidemic may be earlier than usual, and that new coronavirus infections may occur simultaneously.
- The main factors affecting the number of infected people include the following.
- [Vaccination and immunity from infection]
It has become clear that as a certain period elapses after the third vaccination, the infection prevention effect is attenuated compared to the aggravation prevention effect. On the other hand, those in their 60s and older are less likely to acquire immunity by infection than those in their 20s to 40s. It is also pointed out that immunity is attenuated, and there is concern about the spread of infection among elderly people in the future.
- [Contact patterns]
Regarding the nighttime population, the tendency has been flat overall, despite increases in many regions, and while the infection situation is improving in all regions, movements are uneven.
- [Epidemic strain]
After the prevalence of the BA.2 lineage, it has almost been replaced by the BA.5 lineage, which has become mainstream.
- [Climatic factors]
High temperatures are expected to continue in September, and ventilation may be difficult because air conditioning is prioritized.
Status of the medical care provision system
- Nationwide, the burden on the outpatient examination system is evident, and the use rate of beds is decreasing due to the continued improvement of the infection situation, being under 50% in most areas. The use rate of beds for sever cases is also declining. In addition, the numbers of home care recipients and medical treatment adjustments are on a decreasing trend in all areas where the data is available.
- Nationwide, although the burden on the medical care provision system including general medical care partially continues, the situation is improving. On the other hand, in the field of nursing care, patients are being treated in facilities and infection among workers continues.
- Regarding cases of difficulty in emergency transport, the trend of improvement continues nationwide. However, there are still regions with high levels.
Measures to be taken
Basic concepts
- Regarding measures under the Infectious Disease Control Law, appropriate medical care will be provided to the elderly and persons at risk of severe illness, and the period of medical treatment of patients will be reviewed.
- Assuming that a large-scale spread of infection may occur again, each citizen will be asked to take voluntary actions to prevent infection, and the strengthening and prioritization of the health care system will be promoted in order to protect those at high risk of becoming seriously ill, such as the elderly, and to ensure regular medical care.
- The national and local governments will remind the public of the need for routine infection control measures and take measures to support the public's efforts to prevent infection.
- 1. Further promotion of vaccinations
- Preparations must proceed by mid-October for vaccination with the "vaccine for the Omicron variant" for all persons aged 12 and over who have completed the first vaccination.
- By mid-October, the vaccine used the 4th vaccination, which is administered for reasons such as a high risk of severe illness, will be switched from the conventional vaccine to the vaccine for the Omicron variant. The vaccination interval was set at 5 months, but it is necessary to consider shortening the vaccination interval in light of overseas trends, and to reach a conclusion by the end of October.
- Those who have not received vaccination will be encouraged to consider getting the initial vaccination as soon as possible.
- For children (ages 5 to 11), booster vaccinations will be promoted along with the initial vaccination.
- 2. Use of tests
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, the national and local governments are required to secure a system that enables testing, and further utilize testing.
- Implement frequent tests (about 2 or 3 times a week for facility workers) for workers at facilities for elderly people.
- Establishment of a self-testing system for fever outpatients should be further promoted, in which patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Promote further utilization of antigen qualitative test kits, such as by online sales through OTC.
- 3. Securing a medical care provision system
Prefectural governments must take measures to avoid overcrowding of beds and fever outpatient sections with the support of the national government.
- In addition to facilitating the use of available hospital beds and developing temporary medical facilities to supplement hospital beds, making efforts to avoid a shortage of hospital beds and emergency medical care, such as utilization of lodging facilities and resting beds
- Making appropriate adjustments so that patients requiring inpatient treatment can be hospitalized preferentially, performing frequent tests at facilities for elderly people, etc., and further strengthening medical support
- Securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule
- Promotion of effective and less burdensome measures against infection, such as flexible and efficient use of hospital beds through zoning of each hospital room
- Expansion and promotion of fever outpatient services, including the use of online medical care, etc.
- Establishment of a self-testing system for fever outpatients should be further promoted, in which patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Local residents should be informed that they should refrain from visiting an emergency outpatient unit only to receive a precautionary examination without symptoms, according to the actual situation in the region. In addition, in order to respond to concerns and questions at the time of worsening physical conditions, the consultation service by healthcare professionals via telephone should be thoroughly publicized, and this service should also be strengthened.
- Ensuring that workplaces and schools do not require test certificates at the start of medical treatment
- 4. Change of thinking about medical treatment and review of all-case notification
- In reviewing the nationwide notification of all cases, the health care system will be strengthened and prioritized to protect those who are at high risk of becoming seriously ill, and it is necessary to establish an environment where young people with mild symptoms who are not subject to notification can be assured of treatment at home.
- 5. Review of home care period
- Since the risk of infection remains in the shortened period of home care for those who test positive, they should monitor their own physical condition, such as measuring temperature, and take thorough measures against infection when going out. In addition, they must be asked to avoid contact with people who are at risk of becoming seriously ill, such as the elderly.
- To allow the minimum necessary outings, such as shopping for groceries, after 24 hours have passed since symptoms have subsided or when there are no symptoms, it is necessary to take voluntary actions to prevent infection, such as wearing a mask when going out or coming into contact with people, keeping contact with people to a short period of time, and not using public transportation.
- 6. Surveillance
- Deterioration of the accuracy of current surveillance is a concern due to the limited scope of notification, prioritization of notification items, delays in testing and diagnosis/reporting due to many infections, and changes in healthcare-seeking behavior. It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status.
It is also necessary to continue monitoring the trends of variants through genomic surveillance.
- Deterioration of the accuracy of current surveillance is a concern due to the limited scope of notification, prioritization of notification items, delays in testing and diagnosis/reporting due to many infections, and changes in healthcare-seeking behavior. It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status.
- 7. Effective ventilation
Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, it is necessary to publicize and recommend effective ventilation methods to prevent insufficient ventilation due to the use of air conditioners (how to create airflow considering aerosols, installation of partitions that do not block airflow, etc.).
- 8. Re-inspection and implementation of basic infection control
Re-inspection and implementation of the following basic infection control measures are needed.
- Continue proper wearing of nonwoven masks, hand hygiene, thorough ventilation, etc.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, or loud voices.
- Eating and drinking should be done with as few people as possible, and masks should be worn except while eating and drinking.
- People with symptoms such as sore throat, cough, and fever should refrain from going out.
- Refer to guidelines for hospital visits and use of an ambulance.
- To reduce the chances of contact as far as possible, it is necessary for measures at the workplace, such as again promoting the use of telework.
- Organizers of events, meetings, and such should fully evaluate the epidemic situation and risk of infection in the area, and consider whether or not to hold the meeting, and if it is held, measures should be taken to minimize the infection risk.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is considered to have occurred via the same routes as before (droplets adhering to mucosa, aerosol inhalation, contact infection, etc.).
- [Severity]
It has been suggested that infection with the Omicron variant presents a lower risk of hospitalization or aggravation than the Delta variant. However, analyses to date show that the fatality due to infection with the Omicron variant is higher than that due to seasonal influenza. It is also suggested that the incidence of pneumonia is higher than that of seasonal influenza, but given the limited data, it needs to be investigated by various analyses. In the death toll from the previous outbreak compared to last summer's outbreak, it is reported that there are many cases in which the new coronavirus infection is not the direct cause of death, for example, people who have been in a facility for the elderly before the infection are infected and die due to the worsening of the underlying disease. In the current spread of infection, the rate of severe cases has continued to decrease and the ratio of elderly people among hospitalized patients has increased compared to the previous summer, following the previous outbreak. Among the deaths in this outbreak, mechanical ventilation/nasal high flow use rates and steroid prescription rates have decreased compared to the previous outbreak.
- [Virus shedding period]
According to Japanese data, risk of infection remains until 10 days after onset, and infectivity is high until 7 days after onset. Even after waiting for 5 days, 1/3 of patients are still shedding infectious viruses. On Day 8 (after waiting 7 days), most patients (approximately 85%) had not shed infectious virus, and it was reported that even in those who shed the virus, the amount of virus decreased to one-sixth after 7 days compared to the initial stage.
- [Vaccine effect]
For infection with the Omicron variant, the preventive effects of a first vaccination against infection and disease onset are markedly reduced. Its preventive effect on hospitalization is reported to be maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing effect, onset-preventing effect, and hospitalization-preventing effect against infection by the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Regarding the fourth vaccination, it has been reported that while the preventive effect against aggravation was not reduced for 6 weeks, the preventive effect against infection lasted only for a short time.
- [Sublineages of the Omicron variant]
Worldwide, the proportion of the BA.5 lineage is increasing while the number of positive cases increases, suggesting that this lineage is superior to the BA.2 lineage in terms of causing an increase in the number of infected people, but currently the number of positive cases is decreasing. The BA.5 lineage has shown a tendency to escape existing immunity compared with the BA.1 and BA.2 lineages, but no clear findings on the infectivity have been shown. The effective reproduction number of the BA.5 lineage calculated based on the data of Tokyo was about 1.27 times that of BA.2. It was also estimated that it was about 1.3 times higher in samples collected from private testing institutions nationwide.
According to the WHO report, the severity of BA.5 lineage shows both increased and unchanged data compared to the existing Omicron variants, and continued information collection is needed. In addition, the pathogenicity of the BA.5 lineage is reportedly higher than that of the BA.1 and BA.2 lineages, based on Japanese laboratory data, but it has not been confirmed clinically at this time. Although it is unknown whether it is due to the traits of the BA.5 lineage, it should be noted that the numbers of inpatient cases and severe cases are increasing in countries where the number of infected people is increasing mainly in the BA.5 lineage. According to genomic surveillance in Japan, the detection rate of the BA.5 lineage has increased, and the previous dominant variant has largely been replaced with this lineage.
In addition, the BA.2.75 lineage, which has been reported mainly in India since June, and the BA.4.6 lineage reported mainly in the US and UK, have been detected in Japan. However, no clear findings have been obtained overseas regarding its infectivity or severity, compared with other lineages. It is necessary to continue to collect and analyze the situation and findings in other countries regarding these characteristics of the virus, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)
- Details
98th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (September 7, 2022) Material 1
Evaluation of the latest infectious status, etc.
Overview of infection status
- The number of new cases of infection nationwide (by date of report) was approximately 681 per 100,000 in the last week, steadily decreasing at a ratio of this week to last week of 0.69. However, nationwide the level of infections remains higher than the peak in February this year, and the decrease in the number of infections has slowed down in some regions. Attention should be paid to the impact of the re-opening of schools after the summer break on the infection status.
- With the decreasing number of new cases of infection, the number of patients receiving treatment is also decreasing. In addition, the use rate of beds is showing a downward trend, though it is still at a high level nationwide.
The medical care provision system still suffers from the burden, not only of COVID-19, but also general medical services, but the status has improved.
The number of severe patients has turned to show a decreasing trend, and although the number of deaths has stopped to increase, it is remaining high.Effective reproduction number: On a national basis, the most recent number is 0.93 (as of August 21), while the figure stands at 0.92 both in the Tokyo metropolitan and Kansai areas.
Local trends
* The value for new cases of infection is the number of persons per 100,000 among the total number for the latest week, based on the reporting dates.
- Hokkaido
The number of new cases of infection was approximately 644 (approximately 623 in Sapporo City), with a ratio to the previous week of 0.88. Infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 30%.
- North Kanto
In Ibaraki, Tochigi, and Gunma, the numbers of new cases of infection were roughly 559, 524, and 571, with ratios to the previous week of 0.68, 0.79, and 0.75, respectively. In Ibaraki, Tochigi, and Gunma, new cases of infection were mainly in their 30s or younger. The use rates of beds are slightly more than 50% in Ibaraki and slightly more than 40% in Tochigi and Gunma
- Tokyo metropolitan area (Tokyo and 3 neighboring prefectures)
The number of new cases of infection in Tokyo was approximately 579, with a ratio to the previous week of 0.66. Infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 40%, and the use rate of beds for severe cases is slightly less than 30%. In Saitama, Chiba, and Kanagawa, the numbers of new cases of infection were approximately 557, 542, and 441, with ratios to the previous week of 0.73, 0.75, and 0.71, respectively. The use rates of beds are slightly more than 50% in Saitama and Kanagawa and slightly less than 50% in Chiba.
- Chukyo/Tokai
The number of new cases of infection in Aichi was approximately 800, with a ratio to the previous week of 0.71. Infected individuals are mainly in their 30s or younger. The use rate of beds is slightly less than 80%. In Gifu, Shizuoka, and Mie, the numbers of new cases of infection were approximately 795, 659, and 824, with ratios to the previous week of 0.73, 0.68, and 0.70, respectively. The use rates of beds are slightly less than 50% in Gifu, approximately 50% in Shizuoka, and slightly more than 50% in Mie.
- Kansai area
The number of new cases of infection in Osaka was approximately 757, with a ratio to the previous week of 0.66. Infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 50%, while the use rate of beds for severe cases is approximately 10%. In Shiga, Kyoto, Hyogo, Nara, and Wakayama, the numbers of new cases of infection were about 779, 774, 758, 700, and 701, with ratios to the previous week of 0.68, 0.72, 0.68, 0.62, 0.63, respectively. The use rates of beds are approximately 70% in Shiga, slightly more than 50% in Kyoto and Hyogo, approximately 50% in Wakayama, and approximately 40% in Nara.
- Kyushu
The number of new cases of infection in Fukuoka was approximately 772, with a ratio to the previous week of 0.62. Infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 60%. In Saga, Nagasaki, Kumamoto, Oita, Miyazaki, and Kagoshima, the numbers of new cases of infection were approximately 820, 966, 816, 784, 973, and 1,036, with ratios to the previous week of 0.61, 0.61, 0.66, 0.68, 0.64, and 0.66, respectively. The use rates of beds are slightly more than 40% in Saga, approximately 40% in Miyazaki, and slightly more than 50% in Nagasaki, Kumamoto, Oita, and Kagoshima.
- Okinawa
The number of new cases of infection was approximately 820, with a ratio to the previous week of 0.62. Infected individuals are mainly in their 30s or younger. The use rate of beds is slightly less than 60%, while the use rate of beds for severe cases is approximately 50%.
- Areas other than the above
The ratios to the previous week in Iwate, Yamagata, and Fukushima were 0.80, 0.88, and 0.83, respectively. The use rate of beds is slightly more than 60% in Aomori, approximately 60% in Tokushima, slightly less than 60% in Kagawa, and slightly more than 50% in Yamagata, Toyama, Nagano, Hiroshima, and Yamaguchi.
Infection status and future outlook
Infection status
- The number of new cases of infection still indicates a high level of infection nationwide, but it is steadily decreasing in all regions. The level of infection is below the peak at the beginning of February this year in the Tokyo metropolitan and Kansai areas. On the other hand, the level of infection remains higher than the peak of February in many of the other regions, and the decrease in the number of infections has slowed down mainly in northern Japan. In addition, there are still mass infections in facilities for elderly people and medical institutions. The nationwide emergence of new cases of infection and close contacts also continues to affect not only medical institutions and welfare facilities, but also social activities as a whole.
- The number of new cases of infection in each age group started to decrease nationwide; the extent of the decrease in new cases of infection among young people has grown among those in their 20s since last week. The number of new cases of infection among elderly people is also showing a downward trend, and the number of severe cases has recently began to decrease. On the other hand, the increase in the number of deaths has stopped but remained around the record-high level.
- As for the place of new infections, the proportion of home remains unchanged in all age groups, but is increasing especially among people in their 20s. The decreasing trend of school changed and the number of infections is increasing after the start of schools after the vacation (it should be noted that only some of the infection routes [~13%] have been detected because of prioritized active epidemiological surveillance).
Future outlook and factors that increase and suppress infection
- Regarding the future infection status, the decreasing trend in the number of infections may continue in many regions despite regional differences and uncertainty, based on the epi curve of the date of onset and short-term forecast in large cities. On the other hand, the decreasing pace may slow down and the trend may be reversed in some regions because schools started after the break of the summer vacation. The improvement in infection status is expected to relieve medical care provision systems under severe conditions.
- The main factors affecting the number of infected people include the following.
- [Vaccination and immunity from infection]
It has become clear that as a certain period elapses after the third vaccination, the infection prevention effect is attenuated compared to the aggravation prevention effect. On the other hand, those in their 60s and older are less likely to acquire immunity by infection than those in their 20s to 40s. It is also pointed out that immunity is attenuated, and there is concern that the infection will spread among elderly people in the future.
- [Contact patterns]
The nighttime population curve generally remains flat, and has lately decreased to a large extent, especially in Okinawa. These trends may be due to adverse weather conditions.
- [Epidemic strain]
After the prevalence of the BA.2 lineage, it has almost been replaced by the BA.5 lineage, which has become mainstream.
- [Climatic factors]
Since hot weather is expected to continue for some time in September, the preference for using air conditioners may lead to poor ventilation.
Status of the medical care provision system
- Nationwide, there is a burden on the outpatient examination system, but the use rate of beds shows a decreasing trend, though it is still at a high level nationwide, and regions with rates below 50% are also increasing. The usage rate of beds for severe cases in Okinawa is 50%, but it is decreasing in many regions. In addition, the number of home care recipients and medical treatment adjustments is decreasing in almost all regions.
- There is still a burden on the medical care provision system including general medical services, but the status has somewhat improved. On the other hand, in the field of nursing care, many patients are being treated in facilities, and infection is still spreading among patients and workers.
- Although the number of cases with difficulty to find emergency transportation is decreasing nationwide, some regions still show high levels, and caution should be paid to them.
Measures to be taken
Basic concepts
- While the infection situation has not been under control, the possibility of contact with a risk of infection should be minimized based on the facts that the Japanese society have already learned.
To maintain socio-economic activities, everyone has to take measures to prevent infecting others and being infected. - To this end, the national and local governments will remind the public of the need for routine infection control measures, and take measures to support the public's efforts to prevent infection. In addition, efforts must be made to reduce the number of infected people so as not to increase the numbers of severe cases and deaths, as much as possible. Furthermore, further efforts should be made to reinforce the medical care provision system, and reduce the burdens on medical institutions and public health centers.
- 1. Further promotion of vaccinations
- In a case-control study investigating the efficacy of the SAR-CoV-2 vaccine in Japan, the prophylactic effect against the disease at 5 months after the second vaccination was low compared to unvaccinated cases in the epidemic period of BA.5. On the other hand, 3 doses of vaccination (booster) were shown to possibly increase the prophylactic effect against the disease to a moderate to high degree. It was preliminarily reported that the relative efficacy rate of 3 doses of vaccination compared with 2 doses can be expected to a certain extent.
- Concerning “vaccine for the omicron variant,” it is planned to start vaccination of all persons aged 12 years and older who have completed the initial vaccination (first and second dose) around the middle of October, and of those eligible for the fourth vaccination for such reasons as high risk of aggravation of the disease around the middle of September by partial acceleration of the import of the vaccine and using available vaccines for domestic delivery as it becomes available.
- For the fourth vaccination, it is necessary to continue efforts to provide earlier vaccination for eligible persons (elderly people aged 60 years and older, and those aged less than 60 years at risk for severe illness, etc.) for prophylaxis against exacerbation. Based on the local infection status, vaccination should be promoted among workers in medical institutions and elderly care facilities where people at high risk of severe disease are gathered.
- Vaccination with recombinant protein may be selected for up to the third vaccination. It has been confirmed that a third vaccination restores the attenuation over time, of both the preventive effect against the Omicron variant and that against aggravation conferred by the first vaccination. Considering the current infection status, it is necessary to promote consideration of the first and third vaccinations at the earliest possible time.
- Regarding vaccination of children (5-11 years old), the Immunization and Vaccine Section Meeting considered that it was appropriate to impose an obligation to make efforts to vaccinate children, as a certain level of knowledge has been acquired during the spread of the Omicron variant. In addition, the Meeting considered it appropriate to perform additional vaccination.
- 2. Use of tests
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, the national and local governments are required to secure a system that enables testing, and further utilize testing.
- At facilities for elderly people, frequent tests of workers (approximately 2 or 3 times a week) should be performed. Depending on the circumstances in the area, testing on appropriate occasions is recommended for users of facilities.
- Depending on the circumstances in the area, if a cluster occurs it is necessary to carry out frequent testing of teachers and staff at nursery schools and kindergartens.
- At the discretion of local governments and schools, it is necessary to thoroughly observe children’s health, and test those with any symptoms.
- Preliminary testing is further recommended when having a meal with a large number of people or when interacting with elderly people.
- Establishment of a self-testing system for fever outpatients should be further promoted, in which patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- In order to promote these efforts, it is important for the government to provide a stable supply including distribution, by purchasing antigen qualitative test kits, distributing them to prefectural governments, and providing coordination support.
- It is necessary to further promote the utilization of antigen qualitative test kits as OTC through internet sales.
- 3. Effective ventilation
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, effective methods of ventilation should be announced and encouraged to ensure that the use of air conditioners does not lead to poor ventilation (how to create air flow in consideration of aerosols, installation of a partition that does not block the air flow, etc.).
- 4. Securing a medical care provision system
- With support of the national government, local governments are required to take measures to keep the following hospital beds, fever clinics, etc. from being overcrowded.
- In addition to facilitating the use of available hospital beds and developing temporary medical facilities to supplement hospital beds, making efforts to avoid a shortage of hospital beds and emergency medical care, such as utilization of lodging facilities and resting beds.
- Making appropriate adjustments so that patients requiring inpatient treatment can be hospitalized preferentially, performing frequent tests at facilities for elderly people, etc., and further strengthening medical support.
- Securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule.
- Promotion of effective and less burdensome measures against infection, such as flexible and efficient use of hospital beds through zoning of each hospital room.
- Promotion of a basic strategy that is uniformly introduced nationwide to reduce the burden on fever clinics and public health centers, through an emergency measure that makes it possible to limit the scope of notifications of occurrence in regions where fever clinics and public health centers are under extreme pressure.
- Promotion of the expansion and publicity of fever clinics, including the use of online medical services, etc.
- Further promotion of the “self-testing system at fever clinics” to allow symptomatic people to test themselves using a qualitative antigen test kit and, if positive, promptly undergo health monitoring at a Health Follow-up Center, etc. In particular, in regions where fever clinics are under pressure and with a limited scope for notification of occurrence, reinforcement of self-testing in fever clinics should be promoted, such as by reinforcing Health Follow-up Centers.
- Consideration to making announcements to residents depending on their local situations, and in such a manner that they will not refrain from seeking medical care, for example, when residents are asked not to be tested if they are asymptomatic. Announcements about and reinforcement of telephone consultation services for residents are also required to express concerns and questions and be answered by a medical professionals, for example when their condition is worsening.
- Response to emergency cases that are difficult to transport. Confirm the system of accepting patients other than those with COVID-19, and spread awareness of the prevention of heat stroke.
- Establishing and reinforcing a system that allows patients to receive a therapeutic drug appropriately and without delay through publication of the drug’s registration status at clinics/medical institutions
- Ensuring that workplaces and schools do not require test certificates at the start of medical treatment
- Inspecting and securing an oxygen administration system for patients who temporarily need oxygen administration, such as by securing oxygen concentrators, depending on the patient’s condition of home care, arranged accommodation for care, or elderly-care facilities.
- 5. Surveillance
- The limited scope of notification of occurrence, notified items, delay in testing/diagnosis/reporting due to the many cases of the infection, changes in medical care-seeking behavior, etc. are raising concerns about deterioration of the current surveillance program’s accuracy. To understand the epidemiological status, an effective and appropriate surveillance program should be developed promptly.
It is also necessary to monitor the trends of variants through genomic surveillance.
- The limited scope of notification of occurrence, notified items, delay in testing/diagnosis/reporting due to the many cases of the infection, changes in medical care-seeking behavior, etc. are raising concerns about deterioration of the current surveillance program’s accuracy. To understand the epidemiological status, an effective and appropriate surveillance program should be developed promptly.
- 6. Re-inspection and implementation of basic infection control
Re-inspection and implementation of the following basic infection control measures are needed.
- Continue proper wearing of nonwoven masks, hand hygiene, thorough ventilation, etc.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, or loud voices.
- Eating and drinking should be done with as few people as possible, and masks should be worn except while eating and drinking.
- People with symptoms such as sore throat, cough, and fever should refrain from going out.
- Refer to guidelines for hospital visits and use of an ambulance.
- To reduce the chances of contact as far as possible, it is necessary for measures at the workplace, such as again promoting the use of telework.
- Organizers of events, meetings, and such should fully evaluate the epidemic situation and risk of infection in the area, and consider whether or not to hold the meeting, and if it is held, measures should be taken to minimize the infection risk.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is considered to have occurred via the same routes as before (droplets adhering to mucosa, aerosol inhalation, contact infection, etc.).
- [Severity]
It has been suggested that infection with the Omicron variant presents a lower risk of hospitalization or aggravation than the Delta variant. However, analyses to date show that the fatality due to infection with the Omicron variant is higher than that due to seasonal influenza. It is also suggested that the incidence of pneumonia is higher than that of seasonal influenza, but given the limited data, it needs to be investigated by various analyses. The death toll from the previous outbreak compared to last summer's outbreak had a higher proportion of people aged 80 and over. It is reported that there are many cases in which the new coronavirus infection is not the direct cause of death, for example, people who have been in a facility for the elderly before the infection are infected and die due to the worsening of the underlying disease. Attention should also be paid to worsening of the condition of elderly infected people and infected people with an underlying disease, and to the onset of heart failure and aspiration pneumonia.
- [Duration of viral shedding]
Viral shedding in individuals infected with the Omicron variant decreases over time. In patients with symptoms, it has been shown that the possibility of viral shedding is low from 10 days after the date of onset, and that no shedding is observed after 8 days from the date of diagnosis in those without symptoms.
- [Vaccine effect]
For infection with the Omicron variant, the preventive effects of a first vaccination against infection and disease onset are markedly reduced. Its preventive effect on hospitalization is reported to be maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing effect, onset-preventing effect, and hospitalization-preventing effect against infection by the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Regarding the fourth vaccination, it has been reported that while the preventive effect against aggravation was not reduced for 6 weeks, the preventive effect against infection lasted only for a short time.
- [Sublineages of the Omicron variant]
Worldwide, the proportion of the BA.5 lineage is increasing while the number of positive cases is increasing, suggesting that this lineage is superior to the BA.2 lineage in terms of causing an increase in the number of infected people, but currently the number of positive cases is decreasing. The BA.5 lineage has shown a tendency to escape existing immunity compared with the BA.1 and BA.2 lineages, but no clear findings on the infectivity have been shown. The effective reproduction number of the BA.5 lineage calculated based on the data of Tokyo was about 1.27 times that of BA.2. It was also estimated that it was about 1.3 times higher in samples collected from private testing institutions nationwide.
According to the WHO report, the severity of BA.5 lineage shows both increased and unchanged data compared to the existing Omicron variants, and continued information collection is needed. In addition, the pathogenicity of the BA.5 lineage is reportedly higher than that of the BA.1 and BA.2 lineages, based on Japanese laboratory data, but it has not been confirmed clinically at this time. Although it is unknown whether it is due to the traits of the BA.5 lineage, it should be noted that the numbers of inpatient cases and severe cases are increasing in countries where the number of infected people is increasing mainly in the BA.5 lineage. According to genomic surveillance in Japan, the detection rate of the BA.5 lineage is increasing, and the previous dominant variant was replaced by this lineage.
The BA.2.75 lineage, which has been reported mainly in India since June, and the BA.4.6 lineage, which has been reported mainly in the United States and the United Kingdom, have been detected in Japan. However, no clear findings have been obtained overseas regarding its infectivity or severity, compared with other lineages. It is necessary to continue to collect and analyze the situation and findings in other countries regarding these characteristics of the virus, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)
- Details
97th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (August 31, 2022) Material 1
Evaluation of the latest infectious status, etc.
Overview of infection status
- The nationwide number of new cases of infection (based on the reporting dates) was approximately 985 per 100,000 population in the most recent week and the ratio to the previous week was 0.79. Although the number started to decrease after the upward trend in the last week, a high level of infections is continuing nationwide. Attention should be paid to the impact of the re-opening of schools after the summer break on the infection status.
- As the number of new cases of infection started to decrease, the number of patients receiving treatment also started to decrease. The use rate of beds remains high nationwide.
The medical care provision system is facing many problems such as difficulty to transport emergency cases and the absence of medical personnel, causing a significant burden not only on COVID-19-related services but on the medical provision system including general medical services.
The numbers of severe cases and deaths also remain high. In particular, the number of deaths is continuing to exceed the previous record-high level.Effective reproduction number: The latest number (as of August 14) is 1.03 nationwide, 0.99 in the Tokyo metropolitan area, and 1.00 in the Kansai area.
Local trends
* The value for new cases of infection is the number of persons per 100,000 among the total number for the latest week, based on the reporting dates.
- Hokkaido
The number of new cases of infection was approximately 733 (approximately 722 in Sapporo City), with a ratio to the previous week of 0.79. The infected individuals are mainly in their 30s or younger. The use rate of beds is approximately 40%.
- North Kanto
In Ibaraki, Tochigi, and Gunma, the numbers of new cases of infection were approximately 825, 665, and 762, with ratios to the previous week of 0.88, 0.75, and 0.85, respectively. In Ibaraki, Tochigi, and Gunma, they were mainly in their 30s or younger. The use rates of beds are slightly more than 60% in Ibaraki, slightly less than 50% in Tochigi, and slightly more than 50% in Gunma.
- Tokyo metropolitan area (Tokyo and 3 neighboring prefectures)
The number of new cases of infection in Tokyo was approximately 883, with a ratio to the previous week of 0.72. The infected individuals are mainly in their 30s or younger. The use rate of beds is approximately 50%, while the use rate of beds for severe patients is slightly more than 30%. In Saitama, Chiba, and Kanagawa, the numbers of new cases of infection were approximately 758, 722, and 617, with ratios to the previous week of 0.80, 0.95, and 0.82, respectively. The use rates of beds are slightly more than 60% in Saitama, Chiba, and Kanagawa.
- Chukyo/Tokai
The number of new cases of infection in Aichi was approximately 1,128, with a ratio to the previous week of 0.76. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 70%. In Gifu, Shizuoka, and Mie, the numbers of new cases of infection were roughly 1,092, 962, and 1,169, with ratios to the previous week of 0.78, 0.83, and 0.81, respectively. The use rate of beds is slightly more than 60% in Gifu and Shizuoka, and slightly more than 50% in Mie.
- Kansai area
The number of new cases of infection in Osaka was approximately 1,151, with a ratio to the previous week of 0.72. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 60%, while the use rate of beds for severe patients is slightly more than 10%. In Shiga, Kyoto, Hyogo, Nara, and Wakayama, the numbers of new cases of infection were roughly 1,144, 1,078, 1,117, 1,126, and 1,108, with ratios to the previous week of 0.90, 0.87, 0.81, 0.82, and 0.76, respectively. The use rates of beds are slightly more than 60% in Shiga, Hyogo, and Wakayama, slightly less than 60% in Kyoto, and slightly more than 50% in Nara.
- Kyushu
The number of new cases of infection in Fukuoka was approximately 1,250, with a ratio to the previous week of 0.73. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 70%. In Saga, Nagasaki, Kumamoto, Oita, Miyazaki, and Kagoshima, the numbers of new cases of infection were approximately 1,354, 1,578, 1,235, 1,160, 1,516, and 1,560, with ratios to the previous week of 0.69, 0.84, 0.73, 0.75, 0.79, and 0.80, respectively. The use rates of beds are slightly less than 50% in Saga, slightly more than 60% in Nagasaki, Kumamoto, and Kagoshima, slightly more than 50% in Oita, and slightly more than 40% in Miyazaki.
- Okinawa
The number of new cases of infection was approximately 1,329, with a ratio to the previous week of 0.76. The infected individuals are mainly in their 30s or younger. The use rate of beds is approximately 60%, while the use rate of beds for severe cases is slightly more than 30%.
- Areas other than the above
Aomori, Ishikawa, Tokushima, and Kochi had ratios to the previous week of 1.07, 0.91, 1.01, and 0.91, respectively. The use rates of beds are approximately more than 70% in Aomori, approximately 60% in Nagano, Hiroshima, and Yamaguchi, slightly less than 70% in Tokushima, and slightly more than 60% in Kagawa and Ehime.
Infection status and future outlook
Infection status
- Although the number of new cases of infection started to decrease after the upward trend the previous week following the Obon break, a high level of infections is continuing nationwide, still remaining high in some regions. Outbreaks continue to occur in elderly-care facilities and medical institutions. The nationwide emergence of new cases of infection and close contacts also continues to affect not only medical institutions and welfare facilities, but also social activities as a whole.
- The nationwide number of new cases of infection started to decrease in all age groups. In the 20s, in particular, the number started to decrease after the steep increase the previous week, and the decreasing slope is becoming steeper. Although the number of new cases among elderly people also tended to decrease, the numbers of severe cases and deaths still remain high. In particular, the number of deaths is continuing to exceed the previous record-high level.
- Of the places where new infections occur, the proportion accounted for by home tended to remain unchanged while the proportion accounted for by schools, etc. tended to increase after the previous downward trend. The proportion accounted for by office (workplace) generally tended to increase among people in their 20s to 60s. (It should be noted that the route of infection is not fully established in large cities because of the focused approach of active epidemiological surveillance.)
Future outlook and factors that promote and suppress infection
- The epi curve by date of onset and the short-term forecast in large cities indicate that although there are regional differences and uncertainties, there is a possibility that the trend is turning downward from the plateau, but there is concern that the trend may be turning upward due to the impact of schools that will re-open after the summer break. The level of infection is still high nationwide, and the difficult situation of the medical care provision system is expected to continue.
- The main factors affecting the number of infected cases include the following.
- [Vaccination and immunity from infection]
It has become clear that as a certain period elapses after the third vaccination, the infection prevention effect is attenuated compared to the aggravation prevention effect. On the other hand, those in their 60s and older are less likely to acquire immunity by infection than those in their 20s to 40s. It is also pointed out that immunity is attenuated, and there is concern that the infection will spread among elderly people in the future.
- [Contact pattern]
The nighttime population has remained unchanged nationwide, while it has started to increase in large cities such as Tokyo, Aichi, and Osaka.
- [Epidemic strain]
After the prevalence of the BA.2 lineage, it has almost been replaced by the BA.5 lineage, which has become mainstream.
- [Climatic factors]
Since hot weather is expected to continue for some time in September, the preference for using air conditioners may lead to poor ventilation.
Status of the medical care provision system
- Nationwide, there is a burden on the outpatient examination system, and the use rate of beds remains high nationwide, exceeding 50% in most regions. The use rate of beds for severe cases was below 50% in Tokyo and Osaka, but 50% in Kochi. The numbers of patients in home care and arranged accommodation for care remain high in many regions, but is tending to decrease.
- Nationwide, infection among health care professionals has caused inadequate staffing to continue, prolonging the burden on the medical care provision system, including general medical services. In the field of nursing care, in-facility treatment is often encountered, and infection among patients under treatment and their carers is prolonging the difficult situation.
- The positive test rate tended to decrease, but still remained high, raising concerns about whether people who need to undergo testing, such as those who are symptomatic, can receive the tests appropriately.
- The number of emergency cases that were difficult to transport decreased nationwide, but in some regions the number still remained high, and requires attention.
Continued attention is needed for emergency transportation under the influence of extremely hot weather.
Measures to be taken
Basic concepts
- While the infection situation has not been under control, the possibility of contact with a risk of infection should be minimized based on the facts that the Japanese society have already learned.
To maintain socio-economic activities, everyone has to take measures to prevent infecting others and being infected. - To this end, the national and local governments will remind the public of the need for routine infection control measures, and take measures to support the public's efforts to prevent infection. In addition, efforts must be made to reduce the number of infected people so as not to increase the numbers of severe cases and deaths, as much as possible. Furthermore, further efforts should be made to reinforce the medical care provision system, and reduce the burdens on medical institutions and public health centers.
- 1. Further promotion of vaccinations
- In a case-control study investigating the efficacy of the SAR-CoV-2 vaccine in Japan, the prophylactic effect against the disease at 5 months after the second vaccination was low compared to unvaccinated cases in the epidemic period of BA.5. On the other hand, 3 doses of vaccination (booster) were shown to possibly increase the prophylactic effect against the disease to a moderate to high degree. It was preliminarily reported that the relative efficacy rate of 3 doses of vaccination compared with 2 doses can be expected to a certain extent.
- Regarding the booster vaccination with "vaccine for the Omicron variant," it will be prepared for use after the middle of October this year, targeting those who have completed the initial vaccination.
- For the fourth vaccination, it is necessary to continue efforts to provide earlier vaccination for eligible persons (elderly people aged 60 years and older, and those aged less than 60 years at risk for severe illness, etc.) for prophylaxis against exacerbation. Based on the local infection status, vaccination should be promoted among workers in medical institutions and elderly care facilities where people at high risk of severe disease are gathered.
- Vaccination with recombinant protein may be selected for up to the third vaccination. It has been confirmed that a third vaccination restores the attenuation over time, of both the preventive effect against the Omicron variant and that against aggravation conferred by the first vaccination. Considering the current infection status, it is necessary to promote consideration of the first and third vaccinations at the earliest possible time.
- Regarding vaccination of children (5-11 years old), the Immunization and Vaccine Section Meeting considered that it was appropriate to impose an obligation to make efforts to vaccinate children, as a certain level of knowledge has been acquired during the spread of the Omicron variant.
- 2. Use of tests
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, the national and local governments are required to secure a system that enables testing, and further utilize testing.
- Frequent tests (about 2 or 3 times a week for facility workers) are required for workers at facilities for elderly people.
- Depending on the circumstances in the area, testing at appropriate occasions is recommended for users of facilities for elderly people.
- Depending on the circumstances in the area, if a cluster occurs it is necessary to carry out frequent testing of teachers and staff at nursery schools and kindergartens.
- At the discretion of local governments and schools, it is necessary to thoroughly observe children’s health, and test those with any symptoms.
- Preliminary testing is further recommended when having a meal with a large number of people or when interacting with elderly people.
- Establishment of a self-testing system for fever outpatients should be further promoted, in which patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- In order to promote these efforts, it is important for the government to provide a stable supply including distribution, by purchasing antigen qualitative test kits, distributing them to prefectural governments, and providing coordination support.
- It is necessary to promote the utilization of antigen qualitative test kits as OTC.
- 3. Effective ventilation
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, effective methods of ventilation should be announced and encouraged to ensure that the use of air conditioners does not lead to poor ventilation (how to create air flow in consideration of aerosols, installation of a partition that does not block the air flow, etc.).
- 4. Securing a medical care provision system
- With support of the national government, local governments are required to take measures to keep the following hospital beds, fever clinics, etc. from being overcrowded.
- In addition to facilitating the use of available hospital beds and developing temporary medical facilities to supplement hospital beds, making efforts to avoid a shortage of hospital beds and emergency medical care, such as utilization of lodging facilities and resting beds
- Making appropriate adjustments so that patients requiring inpatient treatment can be hospitalized preferentially, performing frequent tests at facilities for elderly people, etc., and further strengthening medical support
- Securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule
- Promotion of effective and less burdensome measures against infection, such as flexible and efficient use of hospital beds through zoning of each hospital room
- Promotion of a basic strategy that is uniformly introduced nationwide to reduce the burden on fever clinics and public health centers, through an emergency measure that makes it possible to limit the scope of notifications of occurrence in regions where fever clinics and public health centers are under extreme pressure.
- Promotion of the expansion and publicity of fever clinics, including the use of online medical services, etc.
- Further promotion of the “self-testing system at fever clinics” to allow symptomatic people to test themselves using a qualitative antigen test kit and, if positive, promptly undergo health monitoring at a Health Follow-up Center, etc. In particular, in regions where fever clinics are under pressure and with a limited scope for notification of occurrence, reinforcement of self-testing in fever clinics should be promoted, such as by reinforcing Health Follow-up Centers.
- Consideration to making announcements to residents depending on their local situations, and in such a manner that they will not refrain from seeking medical care, for example, when residents are asked not to be tested if they are asymptomatic. Announcements about and reinforcement of telephone consultation services for residents are also required to express concerns and questions and be answered by a medical professionals, for example when their condition is worsening.
- Response to emergency cases that are difficult to transport. Confirm the system of accepting patients other than those with COVID-19, and spread awareness of the prevention of heat stroke.
- Establishing and reinforcing a system that allows patients to receive a therapeutic drug appropriately and without delay through publication of the drug’s registration status at clinics/medical institutions
- Ensuring that workplaces and schools do not require test certificates at the start of medical treatment
- Inspecting and securing an oxygen administration system for patients who temporarily need oxygen administration, such as by securing oxygen concentrators, depending on the patient’s condition of home care, arranged accommodation for care, or elderly-care facilities.
- 5. Surveillance
- The limited scope of notification of occurrence, notified items, delay in testing/diagnosis/reporting due to spreading of the infection, changes in medical care-seeking behavior, etc. are raising concerns about deterioration of the current surveillance program’s accuracy. To understand the epidemiological status, an effective and appropriate surveillance program should be developed promptly.
It is also necessary to monitor the trends of variants through genomic surveillance.
- The limited scope of notification of occurrence, notified items, delay in testing/diagnosis/reporting due to spreading of the infection, changes in medical care-seeking behavior, etc. are raising concerns about deterioration of the current surveillance program’s accuracy. To understand the epidemiological status, an effective and appropriate surveillance program should be developed promptly.
- 6. Re-inspection and implementation of basic infection control
Re-inspection and implementation of the following basic infection control measures are needed.
- Eating and drinking should be done with as few people as possible, and masks should be worn except while eating and drinking.
- Continue proper wearing of nonwoven masks, hand hygiene, thorough ventilation, etc.
- People with symptoms such as sore throat, cough, and fever should refrain from going out.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, or loud voices.
- Refer to guidelines for hospital visits and use of an ambulance.
- To reduce the chances of contact as far as possible, it is necessary for measures at the workplace, such as again promoting the use of telework.
- Organizers of events, meetings, and such should fully evaluate the epidemic situation and risk of infection in the area, and consider whether or not to hold the meeting, and if it is held, measures should be taken to minimize the infection risk.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is considered to have occurred via the same routes as before (droplets adhering to mucosa, aerosol inhalation, contact infection, etc.).
- [Severity]
It has been suggested that infection with the Omicron variant presents a lower risk of hospitalization or aggravation than the Delta variant. However, analyses to date show that the fatality due to infection with the Omicron variant is higher than that due to seasonal influenza. It is also suggested that the incidence of pneumonia is higher than that of seasonal influenza, but given the limited data, it needs to be investigated by various analyses. The death toll from the previous outbreak compared to last summer's outbreak had a higher proportion of people aged 80 and over. It is reported that there are many cases in which the new coronavirus infection is not the direct cause of death, for example, people who have been in a facility for the elderly before the infection are infected and die due to the worsening of the underlying disease. Attention should also be paid to worsening of the condition of elderly infected people and infected people with an underlying disease, and to the onset of heart failure and aspiration pneumonia.
- [Duration of viral shedding]
Viral shedding in individuals infected with the Omicron variant decreases over time. In patients with symptoms, it has been shown that the possibility of viral shedding is low from 10 days after the date of onset, and that no shedding is observed after 8 days from the date of diagnosis in those without symptoms.
- [Vaccine effect]
For infection with the Omicron variant, the preventive effects of a first vaccination against infection and disease onset are markedly reduced. Its preventive effect on hospitalization is reported to be maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing effect, onset-preventing effect, and hospitalization-preventing effect against infection by the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Regarding the fourth vaccination, it has been reported that while the preventive effect against aggravation was not reduced for 6 weeks, the preventive effect against infection lasted only for a short time.
- [Sublineages of the Omicron variant]
Worldwide, the proportion of the BA.5 lineage is increasing while the number of positive cases increases, suggesting that this lineage is superior to the BA.2 lineage in terms of causing an increase in the number of infected people, but recently the number of positive cases has decreased. The BA.5 lineage has shown a tendency to escape existing immunity compared with the BA.1 and BA.2 lineages, but no clear findings on the infectivity have been shown. The effective reproduction number of the BA.5 lineage calculated based on the data of Tokyo was about 1.27 times that of BA.2. It was also estimated that it was about 1.3 times higher in samples collected from private testing institutions nationwide.
According to the WHO report, the severity of BA.5 lineage shows both increased and unchanged data compared to the existing Omicron variants, and continued information collection is needed. In addition, the pathogenicity of the BA.5 lineage is reportedly higher than that of the BA.1 and BA.2 lineages, based on Japanese laboratory data, but it has not been confirmed clinically at this time. Although it is unknown whether it is due to the traits of the BA.5 lineage, it should be noted that the numbers of inpatient cases and severe cases are increasing in countries where the number of infected people is increasing mainly in the BA.5 lineage. According to genomic surveillance in Japan, the detection rate of the BA.5 lineage is increasing, and the previous dominant variant was replaced with this lineage.
In addition, the BA.2.75 lineage, which has been reported mainly in India since June, has been detected in Japan. However, no clear findings have been obtained overseas regarding its infectivity or severity, compared with other lineages. It is necessary to continue to collect and analyze the situation and findings in other countries regarding these characteristics of the virus, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)
- Details
掲載日:2022年9月14日
一部追加:2022年9月15日
国立感染症研究所実地疫学研究センター
同 感染症疫学センター
新型コロナウイルス感染症に罹患し、お亡くなりになった方々とご遺族の皆様に対し、深くお悔やみを申し上げます。
背景・目的
厚生労働省は、新型コロナウイルス(以下、「SARS-CoV-2」という。)感染による重症度等の知見を集積・監視するため、感染症の予防及び感染症の患者に対する医療に関する法律(平成10年法律第114号。)第15条に基づく積極的疫学調査の一環として、「新型コロナウイルス感染症の積極的疫学調査におけるゲノム解析及び変異株PCR検査について(要請)」(令和3年2月5日付け健感発0205第4号厚生労働省健康局結核感染症課長通知。令和4年2月10日一部改正。)及び「B.1.1.529系統(オミクロン株)の感染が確認された患者等に係る入退院及び濃厚接触者並びに公表等の取扱いについて」(令和3年11月30日付け厚生労働省新型コロナウイルス感染症対策推進本部事務連絡。令和4年2月2日一部改正。)において、自治体に対し、重症例及び死亡例についての報告やゲノム解析をこれまで依頼してきた。
今般、感染拡大に伴い、小児の感染者数が増加し1)、小児の重症例、死亡例発生への懸念から、厚生労働省及び国立感染症研究所は、関係学会(日本小児科学会、日本集中治療医学会、日本救急医学会)と協力して、SARS-CoV-2感染後の20歳未満の死亡例(以下、小児等の死亡例という。)について、急性期以降の死亡例も含め幅広く調査対象とし、積極的疫学調査を実施することとした。
本報告は、2022年1月1日から2022年8月31日までに報告された小児等の死亡例に関する暫定的な報告である。
方法
報告された小児等の死亡例のうち、下記2つのうちいずれかを満たす者を調査対象とした。自治体及び医療機関の協力のもと、国立感染症研究所職員及び実地疫学専門家養成コース研修員が、自治体による疫学調査等の資料収集、可能な限り現地に赴き実地においての医療機関での診療録の閲覧、及び医師への聞き取り等の調査(以下、実地調査という。)を実施した。
調査対象とした者:
①発症日(あるいは入院日)が2022年1月1日以降のSARS-CoV-2感染後の20歳未満の急性期の死亡例
②発症日(あるいは入院日)が2022年1月1日以降のSARS-CoV-2感染後の20歳未満の急性期以後に死亡した症例(死因を別原因とした症例。発症からの日数は問わない。)
実地調査における主な調査項目:
年齢、性別、基礎疾患、新型コロナワクチン接種歴、発症日、死亡日、症状/所見、死亡に至る経緯等
結果(暫定)
本調査における2022年8月31日現在の症例の概要、及び実地調査の結果は、以下のとおりであった。症例の収集において、調査対象を上述の①または②を満たす者としたが、報告された症例について①と②を明確に分類することは困難であった。なお、下記の記述内容は個人が特定されないよう配慮した。
〇症例の概要
症例は、2022年8月31日時点で、計41例(年齢:0歳8例(20%)、1-4歳10例(24%)、5-11歳17例(41%)、12-19歳5例(12%)、不明1例(2%)、性別:男性23例(56%)、女性18例(44%)、基礎疾患:あり18例(44%)、なし17例(41%)、不明6例(15%))であった。2022年1月1日(疫学週2021年52週)以降の発症日に基づく報告数を図に示した。症例は、2022年1月から継続的に発生し、疫学週2022年28週(7月11日~7月17日)から増加した。
図.新型コロナウイルス感染後の20歳未満の死亡例の報告数(n=34*; 発症日または入院日が2022年1月1日(疫学週2021年52週)~8月31日(疫学週2022年35週))(2022年8月31日時点)**
*発症日不明の7例を除く
**直近の報告はグラフに反映されにくいため、解釈には注意が必要である。
〇実地調査の結果
41例のうち実地調査が実施できた症例は、2022年8月31日時点で32例であり、このうち、明らかな内因性死亡(外傷を除く疾病による死亡)と考えられたのは29例であった。以下、この29例について述べる(表)。
年齢・年代の内訳は、0歳8例(28%)、1-4歳6例(21%)、5-11歳12例(41%)、12-19歳3例(10%)であった。性別は、男性16例(55%)、女性13例(45%)であった。基礎疾患は、あり14例(48%)、なし15例(52%)であった。2022年8月31日時点での基礎疾患ありの内訳は、中枢神経疾患7例(50%)、先天性心疾患2例(14%)、染色体異常2例(14%)等であった(重複あり)。新型コロナワクチンは、29例のうち接種対象外年齢の者が14例(48%)、接種対象年齢の者が15例(52%)であり、接種対象年齢となる5歳以上の15例では、未接種が13例(87%)、2回接種が2例(13%)であった。接種を受けた2例はともに12歳以上であり、発症日は、最終接種日から最低3ヶ月を経過していた。また、医療機関到着時の症状/所見は、発熱23例(79%)、悪心嘔吐15例(52%)、意識障害13例(45%)、咳嗽9例(31%)、経口摂取不良9例(31%)、痙攣8例(28%)、呼吸困難7例(24%)の順に多かった。医療機関において疑われた死亡に至る主な経緯は、循環器系の異常7例(24%:心筋炎、不整脈等)、中枢神経系の異常7例(24%:急性脳症等)、呼吸器系の異常3例(10%:肺炎、細菌性肺炎等)、その他6例(21%:多臓器不全等)、原因不明6例(21%)であった。急性脳症等の中枢神経系の異常、心筋炎や不整脈等の循環器系の異常によって急激な経過を辿った症例があった。発症日は、29例のうち26例について得られ、発症から死亡までの日数が、中央値4日(範囲:0-74日)、内訳は0-2日が8例(31%)、3-6日が11例(42%)、7日以上が7例(27%)であった。
29例のうち基礎疾患があったと考えられた14例について、年齢・年代の内訳は、5歳未満8例(57%)(うち0歳4例)、5歳以上6例(43%)であった。性別は、男性9例(64%)、女性5例(36%)であった。医療機関到着時の症状/所見は、発熱11例(79%)、呼吸困難7例(50%)、悪心嘔吐6例(43%)、咳嗽5例(36%)、経口摂取不良4例(29%)、痙攣3例(21%)、意識障害3例(21%)であった。医療機関において疑われた死亡に至る主な経緯として、循環器系の異常3例(21%)、呼吸器系の異常3例(21%)、中枢神経系の異常2例(14%)、その他3例(21%)、原因不明3例(21%)であった。発症日は、14例のうち12例について得られ、発症から死亡までの日数は、中央値4日(範囲:1-74日)、内訳は0-2日が3例(25%)、3-6日が7例(58%)、7日以上が2例(17%)であった。
29例のうち基礎疾患がなかったと考えられた15例について、年齢・年代の内訳は、5歳未満6例(40%)(うち0歳4例)、5歳以上9例(60%)であった。性別は、男性7例(47%)、女性8例(53%)であった。医療機関到着時の症状/所見は、発熱12例(80%)、意識障害10例(67%)、悪心嘔吐9例(60%)、痙攣5例(33%)、経口摂取不良5例(33%)、咳嗽4例(27%)、呼吸困難0例(0%)であった。医療機関において疑われた死亡に至る主な経緯は、中枢神経系の異常5例(33%)、循環器系の異常4例(27%)、その他3例(20%)、原因不明3例(20%)であり、呼吸器系の異常はなかった。発症日は、15例のうち14例について得られ、発症から死亡までの日数は、中央値4.5日(範囲:0-15日)、内訳は0-2日が5例(36%)、3-6日が4例(29%)、7日以上が5例(36%)であった。
表. 新型コロナウイルス感染後の20歳未満の死亡例の特性
(n=29 ; 発症日または入院日が2022年1月1日から8月31日、明らかな内因性死亡に限る)(2022年8月31日時点)
* 発症から死亡までの日数は発症日に関する情報が得られた26例(基礎疾患あり12例、基礎疾患なし14例)
考察
2022年8月31日時点における、2022年1月1日から2022年8月31日までに報告された小児等の死亡例、41例について暫定的な報告を行った。症例数は、7月中旬から増加していた。
今回の実地調査で内因性死亡が明らかとされた小児等の死亡例において、基礎疾患のなかった症例も死亡していることから、SARS-CoV-2感染後は、基礎疾患のある者はもちろん、基礎疾患のない者においても、症状の経過を注意深く観察することが必要であると考えられた。新型コロナワクチンは、接種対象でも多くの小児の死亡例では未接種であった。また、症状は、日本小児科学会による国内小児におけるCOVID-19レジストリ調査2)と比較して、呼吸器症状以外の症状のうち、悪心嘔吐(52%)、意識障害(45%)、経口摂取不良(31%)、痙攣(28%)の割合が高かった。新型コロナウイルス感染症における重症度分類は、主に呼吸器症状等により分類されているが3)、小児においては、痙攣、意識障害などの神経症状や、嘔吐、経口摂取不良等の呼吸器症状以外の全身症状の出現にも注意を払う必要があると考えられた。発症から死亡までの日数は、1週間未満が73%を占めており、特に発症後1週間の症状の経過観察が重要であると考えられた。
調査に関する制限と今後
本報告は、2022年8月31日時点での暫定的な報告であり、今後の調査の進捗にあわせて、情報の更新・修正がなされる可能性がある点、及び本調査では、SARS-CoV-2感染と死亡との因果関係を検討していない点に留意する必要がある。引き続き、自治体及び関係学会の協力のもと、本調査を継続していく予定である。
本調査における協力学会:日本小児科学会、日本集中治療医学会、日本救急医学会
謝辞:本調査にご協力いただきました関係者の皆様に心より御礼申し上げます。
参考資料:
1. 厚生労働省 データからわかる-新型コロナウイルス感染症情報
https://covid19.mhlw.go.jp/ (閲覧日:2022年8月19日)
2. 小児科学会 予防接種・感染症対策委員会「データベースを用いた国内発症小児 Coronavirus Disease 2019 (COVID-19) 症例の臨床経過に関する検討」の中間報告:第3報、2022年3月28日
http://www.jpeds.or.jp/uploads/files/20220328_tyukan_hokoku3.pdf
3. 新型コロナウイルス感染症診療の手引き・第8.0版
https://www.mhlw.go.jp/content/000967699.pdf
追加:(2022/9/15)参考資料1.の引用表記を追記しました。
- Details
96th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (August 24, 2022) Material 1
Evaluation of the latest infectious status, etc.
Overview of the infection status
- The number of new cases of infection nationwide (based on the reporting dates) is approximately 1,250 per 100,000 population for the latest week, and the ratio to the previous week is 1.19, which is an increase from last week's downward trend. The highest number ever as been surpassed, as the highest level of infection continues. Increase was seen in most regions, partly due to the influence of socio-economic activities such as Obon and summer vacation.
- As the number of new cases of infection start to increase, the number of patients receiving treatment is also starting to increase. In addition, the use rate of beds is increasing or remains high nationwide. As for the medical care provision system, many cases of difficult emergency transportation and absences of healthcare professionals from work have placed a significant burden not only on treatment for COVID-19, but also on the medical care provision system, including general medical care. There are concerns that the situation will deteriorate further.
In addition, the numbers of severe cases and deaths are on the rise, and there is particular concern that the number of deaths may further increase to exceed the previous record-high.Effective reproduction number: On a national basis, the most recent number is 0.96 (as of August 7), while the figure stands at 0.92 in the Tokyo metropolitan area and 0.94 in the Kansai area.
Local trends
* The value for new cases of infection is the number of persons per 100,000 among the total number for the latest week, based on the reporting dates.
- Hokkaido
The number of new cases of infection was approximately 933 (approximately 957 in Sapporo City), with a ratio to the previous week of 1.07. The infected individuals are mainly in their 30s or younger. The use rate of beds is approximately 40%.
- North Kanto
In Ibaraki, Tochigi, and Gunma, the numbers of new cases of infection were roughly 940, 889, and 900, with ratios to the previous week of 1.31, 1.29 and 1.16, respectively. In Ibaraki, Tochigi, and Gunma, they were mainly in their 30s or younger. The use rates of beds are slightly more than 60% in Ibaraki, slightly less than 70% in Tochigi, and slightly less than 60% in Gunma.
- Tokyo metropolitan area (Tokyo and 3 neighboring prefectures)
The number of new cases of infection in Tokyo was approximately 1,221, with a ratio to the previous week of 0.96. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 50%, while the use rate of beds for severe cases is about 60%. In Saitama, Chiba, and Kanagawa, the numbers of new cases of infection were approximately 946, 764, and 756, with ratios to the previous week of 1.04, 1.06, and 0.94, respectively. The use rate of beds is slightly more than 60% in Saitama and Chiba and slightly more than 70% in Kanagawa.
- Chukyo/Tokai
The number of new cases of infection in Aichi was approximately 1,476, with a ratio to the previous week of 1.34. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 70%. In Gifu, Shizuoka, and Mie, the numbers of new cases of infection were roughly 1,398, 1,165, and 1,449, with ratios to the previous week of 1.31, 1.27, and 1.51, respectively. The use rates of beds are slightly less than 60% in Gifu, approximately 70% in Shizuoka, and slightly more than 50% in Mie.
- Kansai area
The number of new cases of infection in Osaka was approximately 1,601, with a ratio to the previous week of 1.22. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly less than 70%, while the use rate of beds for severe cases is approximately 50%. In Shiga, Kyoto, Hyogo, Nara, and Wakayama, the numbers of new cases of infection were roughly 1,267, 1,240, 1,378, 1,378, and 1,458, with ratios to the previous week of 1.12, 1.04, 1.13, 1.26, and 1.20, respectively. The use rates of beds are approximately 70% in Shiga, and slightly more than 60% in Kyoto, Hyogo, Nara, and Wakayama.
- Kyushu
The number of new cases of infection in Fukuoka was approximately 1,714, with a ratio to the previous week of 1.24. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 70%. In Saga, Nagasaki, Kumamoto, Oita, Miyazaki, and Kagoshima, the numbers of new cases of infection were approximately 1,956, 1,890, 1,697, 1,536, 1,908, and 1,947, with ratios to the previous week of 1.45, 1.33, 1.38, 1.26, 1.20, and 1.27, respectively. The use rates of beds are slightly more than 50% in Saga, Nagasaki, and Miyazaki, slightly more than 60% in Kumamoto and Kagoshima, and slightly less than 60% in Oita.
- Okinawa
The number of new cases of infection was approximately 1,758, with a ratio to the previous week of 0.99. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 70%, while the use rate of beds for severe patients is slightly more than 30%.
- Areas other than the above
The ratios to the previous week in Akita, Yamagata, Fukushima, Toyama, Shimane, Tokushima, Ehime, and Kochi are 1.61, 1.46, 1.45, 1.56, 1.53, 1.79, 1.43, and 1.41, respectively. The use rates of beds are slightly more than 80% in Aomori, slightly more than 60% in Niigata and Okayama, slightly less than 70% in Nagano and Ehime, and slightly more than 70% in Hiroshima.
Infection status and future outlook
Infection status
- The number of new cases of infection increased in most regions, partly due to the increase in socio-economic activities such as Obon and summer vacation. In many regions and nationwide, the highest infection levels continue, surpassing all-time highs. In addition, there are some regions where the number once tended to decrease or remained high, in which rapid increase continues. On the other hand, in Tokyo, Kanagawa, and Okinawa, a decreasing trend can also be seen. In addition, the number of “patients receiving treatment within facilities” has actually been increasing due to a rapid increase in mass infections at facilities for elderly people and shortages of beds. In addition, the rapid increase in cases of infection and close contacts nationwide is still affecting not only medical institutions and welfare facilities, but also social activities as a whole.
- The number of new cases of infection in each age group started to increase nationwide, except among those under the age of 10, with a particularly large increase among those in their 20s. On the other hand, as the trend was before, increases in the number of severe cases and deaths tend to lag behind the rapid increase in the number of new infections. The number of deaths in particular continue to rapidly increase, and there is concern that there will be a further increase in the number of deaths in the future that will exceed the previous record-high number.
- Regarding the place of contracting new infections, the rate of infections that develop at home is still showing an increasing trend, while at schools the trend is changing from decrease to increase. In addition, the percentage of people who contracted the infection at the office (workplace) has increased among people in their 20s to 60s. (It must be kept in mind that active epidemiological surveillance is focused on large cities, and that infection routes are not fully understood).
Future outlook and factors that increase and suppress infection
- Regarding future infection status, the number of new infections may continue to increase or remain high in many regions, based on the epi curve of the date of onset and short-term forecast in large cities. There is also concern about the effects of the reopening of schools after the summer vacation. The number of infected people is unlikely to decrease soon, and the severe situation in the medical care system is expected to continue.
- The main factors affecting the number of infected people include the following.
- [Vaccination and immunity from infection]
It has become clear that as a certain period elapses after the third vaccination, the infection prevention effect is attenuated compared to the aggravation prevention effect. On the other hand, those in their 60s or older are less likely to acquire immunity by infection than those in their 20s to 40s. It is also pointed out that immunity is attenuated, and there is concern that the infection will spread further among elderly people in the future.
- [Contact patterns]
The nighttime population curve generally remains flat, and in many areas such as Tokyo and Osaka, it tends to decrease.
- [Epidemic strain]
After the prevalence of the BA.2 lineage, it has almost been replaced by the BA.5 lineage, which has become mainstream. The BA.5 lineage is thought to cause an increase the number of infected persons more easily, and there is concern about immune escape, which may be a factor to increase the number of infected persons.
- [Climatic factors]
Although it was late August, the weather was still hot, and ventilation may be difficult because air conditioning is prioritized.
Status of the medical care provision system
- Nationwide, the burden on the outpatient examination system is increasing, and the use rate of beds has increased or remains high nationwide, exceeding 50% in most regions. The use rate of beds for severe patients now exceeds 50% in Tokyo and Osaka. In addition, the numbers of home care recipients and medical treatment adjustments remain high in many regions or continue to increase.
- Sufficient manpower cannot be secured yet due to an increase in infections among healthcare professionals nationwide, including Okinawa. The burden on the medical care provision systems has persisted and includes general medical services. In the field of nursing care too, the difficult situation continues due to the increasing numbers of patients being treated in facilities and infection among workers.
- The positive rate of the test remains high, complicating assessment. There is also concern whether the test is appropriately performed on those who need it, such as symptomatic people.
- Although the number of cases of difficulty in emergency transport has decreased nationwide, such cases have increased in some regions and caution should be paid to them. In addition, careful attention should be paid to the increase in cases of ambulance transportation due to the effects of the continuing hot weather.
Measures to be taken
Basic concepts
- In the midst of the spread of infection, it is necessary to reduce, as much as possible the chances of contacts that risk infection, based on the various knowledge that Japanese society has already learned.
Also, in order to maintain socio-economic activities, it is necessary to work on methods for people to avoid infecting and being infected. - To this end, the national and local governments will remind the public of the need for routine infection control measures, and take measures to support the public's efforts to prevent infection. In addition, efforts must be made to reduce the number of infected people so as not to increase the numbers of severe cases and deaths, as much as possible. Furthermore, further efforts should be made to reinforce the medical care provision system, and reduce the burdens on medical institutions and public health centers.
- 1. Further promotion of vaccinations
- In a case-control study investigating the efficacy of the SAR-CoV-2 vaccine in Japan, the prophylactic effect against the disease at 5 months after the second vaccination was low compared to unvaccinated cases in the epidemic period of BA.5. On the other hand, 3 doses of vaccination (booster) were shown to possibly increase the prophylactic effect against the disease to a moderate to high degree. It was preliminarily reported that the relative efficacy rate of 3 doses of vaccination compared with 2 doses can be expected to a certain extent.
- Regarding the booster vaccination with "vaccine for the Omicron variant," it will be prepared for use after the middle of October this year, targeting those who have completed the initial vaccination.
- For the fourth vaccination, it is necessary to continue efforts to provide earlier vaccination for eligible persons (elderly people aged 60 years and older, and those aged less than 60 years at risk for severe illness, etc.) for prophylaxis against exacerbation. Considering the ongoing spread of infection, workers at medical institutions, facilities for elderly people, etc. where many individuals who are at high risk of becoming severely ill gather, have also been included in those who are eligible for vaccination.
- Vaccination with recombinant protein may be selected for up to the third vaccination. It has been confirmed that a third vaccination restores the attenuation over time, of both the preventive effect against the Omicron variant and that against aggravation conferred by the first vaccination. Considering the current infection status, it is necessary to promote consideration of the first and third vaccinations at the earliest possible time.
- Regarding vaccination of children (5-11 years old), the Immunization and Vaccine Section Meeting considered that it was appropriate to impose an obligation to make efforts to vaccinate children, as a certain level of knowledge has been acquired during the spread of the Omicron variant.
- 2. Use of tests
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, the national and local governments are required to secure a system that enables testing, and further utilize testing.
- Frequent tests (about 2 or 3 times a week for facility workers) are required for workers at facilities for elderly people.
- Depending on the circumstances in the area, testing at appropriate occasions is recommended for users of facilities for elderly people.
- Depending on the circumstances in the area, if a cluster occurs it is necessary to carry out frequent testing of teachers and staff at nursery schools and kindergartens.
- At the discretion of local governments and schools, it is necessary to thoroughly observe children’s health, and test those with any symptoms.
- Preliminary testing is further recommended when having a meal with a large number of people or when interacting with elderly people.
- Establishment of a self-testing system for fever outpatients should be further promoted, in which patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- In order to promote these efforts, it is important for the government to provide a stable supply including distribution, by purchasing antigen qualitative test kits, distributing them to prefectural governments, and providing coordination support.
- It is necessary to promote the utilization of medical antigen qualitative test kits as OTC.
- 3. Effective ventilation
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, it is necessary to publicize and recommend effective ventilation methods in the summer when ventilation becomes insufficient due to the use of air conditioners (how to create airflow considering aerosols, installation of partitions that do not block airflow, etc.).
- 4. Securing a medical care provision system
- In preparation for further spread of infection, prefectural governments must take measures to avoid overcrowding of beds and fever outpatient sections with the support of the national government.
- In addition to facilitating the use of available hospital beds and developing temporary medical facilities to supplement hospital beds, making efforts to avoid a shortage of hospital beds and emergency medical care, such as utilization of lodging facilities and resting beds
- Making appropriate adjustments so that patients requiring inpatient treatment can be hospitalized preferentially, performing frequent tests at facilities for elderly people, etc., and further strengthening medical support
- Securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule
- Promotion of effective and less burdensome measures against infection, such as flexible and efficient use of hospital beds through zoning of each hospital room
- Establishment of a self-testing system for fever outpatients should be further promoted, in which patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Strengthening of the supply system of the antigen qualitative test kits, and understanding and publicizing the cases of home care without going through a fever outpatient section
- Local residents should be informed that they should refrain from visiting an emergency outpatient unit only to receive a precautionary examination without symptoms, according to the actual situation in the region. In addition, in order to respond to concerns and questions at the time of worsening physical conditions, the consultation service by healthcare professionals via telephone should be thoroughly publicized, and this service should also be strengthened.
- A system of appropriate and early administration of therapeutic drugs should be established and strengthened, such as publication of the registration status of therapeutic drugs in medical care/testing institutions.
- Response to ambulance transport difficulties In addition to confirming the acceptance system for patients other than those with COVID-19, spreading awareness of heat stroke prevention and warning of increased emergency transportation due to heat stroke.
- Ensuring that workplaces and schools do not require test certificates at the start of medical treatment
- Further promote the reduction of burdens, such as hospitalization coordination and outsourcing/unification of operations by the hospitalization coordination division, so that public health center operations will not be strained.
- Inspecting and securing oxygen administration systems for patients who temporarily need oxygen administration, such as securing oxygen concentrators, in view of the increase in the numbers of home care recipients and medical treatment adjustments, and medical care in facilities for elderly people.
- 5. Surveillance
- Deterioration of the accuracy of current surveillance is a concern due to prioritization of notification items, delays in testing and diagnosis/reporting due to the spread of infection, and changes in healthcare-seeking behavior. It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status. It is also necessary to continue monitoring the trends of variants through genomic surveillance.
- 6. Re-inspection and implementation of basic infection control
- Re-inspection and implementation of the following basic infection control measures are needed.
- Eating and drinking should be done with as few people as possible, and masks should be worn except while eating and drinking.
- Continue proper wearing of nonwoven masks, hand hygiene, thorough ventilation, etc.
- People with symptoms such as sore throat, cough, and fever should refrain from going out.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, or loud voices.
- Refer to guidelines for hospital visits and use of an ambulance.
- To reduce the chances of contact as far as possible, it is necessary for measures at the workplace, such as again promoting the use of telework.
- Organizers of events, meetings, and such should fully evaluate the epidemic situation and risk of infection in the area, and consider whether or not to hold the meeting, and if it is held, measures should be taken to minimize the infection risk.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is considered to have occurred via the same routes as before (droplets adhering to mucosa, aerosol inhalation, contact infection, etc.).
- [Severity]
It has been suggested that infection with the Omicron variant presents a lower risk of hospitalization or aggravation than the Delta variant. However, analyses to date show that the fatality due to infection with the Omicron variant is higher than that due to seasonal influenza. It is also suggested that the incidence of pneumonia is higher than that of seasonal influenza, but given the limited data, it needs to be investigated by various analyses. The death toll from the previous outbreak compared to last summer's outbreak had a higher proportion of people aged 80 and over. It is reported that there are many cases in which the new coronavirus infection is not the direct cause of death, for example, people who have been in a facility for the elderly before the infection are infected and die due to the worsening of the underlying disease. Attention should also be paid to worsening of the condition of elderly infected people and infected people with an underlying disease, and to the onset of heart failure and aspiration pneumonia.
- [Duration of viral shedding]
Viral shedding in individuals infected with the Omicron variant decreases over time. In patients with symptoms, it has been shown that the possibility of viral shedding is low from 10 days after the date of onset, and that no shedding is observed after 8 days from the date of diagnosis in those without symptoms.
- [Vaccine effect]
For infection with the Omicron variant, the preventive effects of a first vaccination against infection and disease onset are markedly reduced. Its preventive effect on hospitalization is reported to be maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing effect, onset-preventing effect, and hospitalization-preventing effect against infection by the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Regarding the fourth vaccination, it has been reported that while the preventive effect against aggravation was not reduced for 6 weeks, the preventive effect against infection lasted only for a short time.
- [Sublineages of the Omicron variant]
Worldwide, the proportion of the BA.5 lineage is increasing while the number of positive cases increases, suggesting that this lineage is superior to the BA.2 lineage in terms of causing an increase in the number of infected people, but recently the number of positive cases has decreased. The BA.5 lineage has shown a tendency to escape existing immunity compared with the BA.1 and BA.2 lineages, but no clear findings on the infectivity have been shown. The effective reproduction number of the BA.5 lineage calculated based on the data of Tokyo was about 1.27 times that of BA.2. It was also estimated that it was about 1.3 times higher in samples collected from private testing institutions nationwide.
According to the WHO report, the severity of BA.5 lineage shows both increased and unchanged data compared to the existing Omicron variants, and continued information collection is needed. In addition, the pathogenicity of the BA.5 lineage is reportedly higher than that of the BA.1 and BA.2 lineages, based on Japanese laboratory data, but it has not been confirmed clinically at this time. Although it is unknown whether it is due to the traits of the BA.5 lineage, it should be noted that the numbers of inpatient cases and severe cases are increasing in countries where the number of infected people is increasing mainly in the BA.5 lineage. According to genomic surveillance in Japan, the detection rate of the BA.5 lineage is increasing, and the previous dominant variant was replaced with this lineage.
In addition, the BA.2.75 lineage, which has been reported mainly in India since June, has been detected in Japan. However, no clear findings have been obtained overseas regarding its infectivity or severity, compared with other lineages. It is necessary to continue to collect and analyze the situation and findings in other countries regarding these characteristics of the virus, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)
- Details
95th Meeting of the COVID-19 Advisory Board of the Ministry of Health, Labour and Welfare (August 18, 2022) Material 1
Evaluation of the latest infectious status, etc.
Overview of the infection status
- The number of new cases of infection nationwide (based on the reporting dates) is approximately 1,036 per 100,000 population for the latest week, and the ratio to the previous week has decreased to 0.87. The number of infected persons is increasing in some regions, and the highest level of infection ever continues nationwide. On the other hand, in view of the severe pressure on the testing system, changing healthcare-seeking behavior, and the delay in the conduct of tests and examinations and the publication of reports during the summer vacations and Obon holidays; the infection status may still have been underestimated.
- As the number of new cases of infection start to decrease, the number of patients receiving treatment is also starting to decrease. On the other hand, the use rate of beds is increasing or remains high nationwide. As for the medical care provision system, the increasing inability to provide smooth emergency transportation and the absence from work of healthcare workers have not improved, placing a significant burden not only on COVID-19 treatment, but also the medical care provision system in general. There is concern that the situation may deteriorate further.
In addition, the numbers of severe cases and deaths are on the rise, and there is particular concern that the number of deaths may further increase to exceed the previous record-high.Effective reproduction number: On a national basis, the most recent number is 1.00 (as of July 31), while the figure stands at 0.99 both in the Tokyo metropolitan and Kansai areas.
Local trends
* The value for new cases of infection is the number of persons per 100,000 among the total number for the latest week, based on the reporting dates.
- Hokkaido
The number of new cases of infection was approximately 856 (approximately 909 in Sapporo City), with a ratio to the previous week of 0.97. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 40%.
- North Kanto
In Ibaraki, Tochigi, and Gunma, the numbers of new cases of infection were roughly 708, 656, and 755, with ratios to the previous week of 0.75, 0.73, and 0.84, respectively. In Ibaraki, Tochigi, and Gunma, they were mainly in their 30s or younger. The use rates of beds are slightly less than 60% in Ibaraki, slightly more than 60% in Tochigi, and slightly more than 50% in Gunma, respectively.
- Tokyo metropolitan area (Tokyo and 3 neighboring prefectures)
The number of new cases of infection in Tokyo was approximately 1,240, with a ratio to the previous week of 0.82. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly less than 60%, and the use rate of beds for severe patients is slightly more than 60%. In Saitama, Chiba, and Kanagawa, the numbers of new cases of infection were approximately 864, 698, and 772, with ratios to the previous week of 0.77, 0.69, and 0.77, respectively. The use rates of beds are slightly less than 70% in Saitama, slightly more than 60% in Chiba, and slightly more than 70% in Kanagawa, respectively.
- Chukyo/Tokai
The number of new cases of infection in Aichi was approximately 1,102, with a ratio to the previous week of 0.82. The infected individuals are mainly in their 30s or younger. The use rate of beds is approximately 70%. In Gifu, Shizuoka, and Mie, the numbers of new cases of infection were roughly 1,095, 917, and 949, with ratios to the previous week of 0.95, 0.83, and 0.85, respectively. The use rates of beds are slightly more than 50% in Gifu, slightly less than 60% in Mie, and slightly more than 70% in Shizuoka.
- Kansai area
The number of new cases of infection in Osaka was approximately 1,305, with a ratio to the previous week of 0.82. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly more than 60%, while the use rate of beds for severe cases is roughly 50%. In Shiga, Kyoto, Hyogo, Nara, and Wakayama, the numbers of new cases of infection were roughly 1,096, 1,122, 1,179, 1,088, and 1,198, with ratios to the previous week of 0.89, 0.83, 0.86, 0.94, and 0.97, respectively. The use rates of beds are slightly more than 80% in Shiga, approximately 70% in Wakayama, approximately 60% in Kyoto, and slightly more than 60% in Hyogo and Nara, respectively.
- Kyushu
The number of new cases of infection in Fukuoka was approximately 1,350, with a ratio to the previous week of 0.86. The infected individuals are mainly in their 30s or younger. The use rate of beds is slightly less than 80%. In Saga, Nagasaki, Kumamoto, Oita, Miyazaki, and Kagoshima, the numbers of new cases of infection were approximately 1,470, 1,418, 1,273, 1,273, 1,581, and 1,578, with ratios to the previous week of 1.07, 1.04, 0.85, 1.06, 1.01, and 1.07, respectively. The use rates of beds are slightly more than 50% in Saga, Oita, and Miyazaki, slightly less than 60% in Nagasaki, approximately 70% in Kumamoto, and slightly more than 60% in Kagoshima.
- Okinawa
The number of new cases of infection was the highest nationwide at approximately 1,753, with a ratio to the previous week of 0.80. The infected individuals are mainly in their 30s or younger. The use rate of beds is approximately 90%, while the use rate of beds for severe patients is slightly more than 30%.
- Areas other than above
The ratio to the previous week in Yamagata, Yamaguchi, Tokushima, Kagawa, Ehime, and Kochi is 1.17, 1.15, 1.19, 1.15, 1.12, and 1.16, respectively. The use rates of beds are slightly more than 60% in Aomori, Okayama, and Hiroshima, approximately 60% in Niigata and Nagano, and approximately 70% in Ishikawa
Infection status and future outlook
Infection status
- Concerning the number of new cases of infection, the effects of reducing the number of tests during the summer vacation and the Obon holidays, and voluntary care at home should be carefully monitored. The number of infected persons is taking a downward trend mainly in the Tokyo metropolitan area and it started to decrease nationwide, but is still at the highest level of infection ever. In addition, the number of infected persons is increasing in some regions, and there are some regions where the number once tended to decrease or remained high, where a rapid increase has been seen. In Okinawa, the infection is showing a downward trend but at a higher level than in other regions; medical care services are under much pressure. In addition, the number of “patients receiving treatment within facilities” has actually been increasing due to a rapid increase in mass infections at facilities for elderly people and shortages of beds. In addition, the rapid increase in cases of infection and close contacts nationwide is still affecting not only medical institutions and welfare facilities, but also social activities as a whole.
- The number of new cases of infection in each age group started to decrease nationwide; the extent of decrease has become larger in young people, mainly in their teens, especially in summer vacation. On the other hand, as the trend was before, increases in the number of severe cases and deaths tend to lag behind the rapid increase in the number of new infections. The number of deaths in particular showed a rapid increase close to the peak level of the sixth wave, and there is concern that there will be a further increase in the number of deaths in the future that will exceed the previous record-high number.
- Regarding the place of contracting new infections, the rate of infections that develop at home is still showing an increasing trend, with a decreasing trend at schools, due to the impact of the summer vacation. In addition, the percentage of people who contracted the infection at the office (workplace) increased among people in their 20s and decreased among those in their 30s to 60s. In addition, the percentage of people who contract it in the hospital is increasing among people in their 50s to 70s (it must be kept in mind that active epidemiological surveillance is focused on large cities, and that infection routes are not fully understood).
Future outlook and factors that increase and suppress infection
- Regarding the future infection status, according to the epi curve of onset dates and the short-term forecasts for large cities, most regions are thought to have passed the peak, and in some areas the number of new infections has actually decreased, although the numbers are still rising or remaining high in quite a number of regions. Effects of movement of people during the Obon holidays is a concern. Much pressure on the medical care provision systems will continue unless the number of infected persons decreases early.
- Factors that affect the number of infected individuals include: (1) the gradual diminishing of the immunity acquired by the third vaccination and infection, (2) possible increase in chances of contact during summer vacations, events and Obon, etc., and (3) the situation that the previously dominant variant has almost been replaced with the Omicron variant of BA.5 lineage.
- [Vaccination]
It has become clear that as a certain period elapses after the third vaccination, the infection prevention effect is attenuated compared to the aggravation prevention effect. In addition, the immunity acquired from previous infections is expected to similarly decline in the future.
- [Contact patterns]
The nighttime population curve generally remains flat. In large cities including the Tokyo metropolitan area and Okinawa, it has decreased or remained flat. There are also some regions where a rapid increase was seen in association with the holding of large festivals, etc.
- [Epidemic strain]
After the prevalence of the BA.2 lineage, it has almost been replaced by the BA.5 lineage, which has become mainstream. The BA.5 lineage is thought to cause an increase the number of infected persons more easily, and there is concern about immune escape, which may be a factor to increase the number of infected persons.
- [Climatic factors]
It is a time when indoor activities increase due to rising temperatures, but ventilation may be difficult because air conditioning is prioritized.
Status of the medical care provision system
- Nationwide, the burden on the outpatient examination system is increasing, and the use rate of beds has increased or remains high nationwide, and regions with rates exceeding 50% are increasing. In particular, the rate exceeds 90% in Okinawa, which is under much pressure. The use rate of beds for severe patients now exceeds 50% in Tokyo and Osaka. On the other hand, the number of patients in home care and arranged accommodation for care are still showing an increasing trend in many regions. In some regions, the rate of increase started to slow down or the trend started to turn downward.
- Sufficient manpower cannot be secured yet due to an increase in infections among healthcare professionals nationwide, including Okinawa. The burden on the medical care provision systems has persisted and includes general medical services. In the field of nursing care too, the difficult situation continues due to the increasing numbers of patients being treated in facilities and infection among workers.
- The positive rate of the test remains high, complicating assessment. There is also concern whether the test is appropriately performed on those who need it, such as people with symptoms.
- Although the increased burden on emergency transportation has generally slowed down, such cases have increased in some regions and caution should be paid to them. In addition, careful attention should be paid to the increase in cases of ambulance transportation due to the effects of the continuing hot weather.
Measures to be taken
Basic concepts
- In the midst of the spread of infection, it is necessary to reduce, as much as possible the chances of contacts that risk infection, based on the various knowledge that Japanese society has already learned. Also, in order to maintain socio-economic activities, it is necessary to work on methods for people to avoid infecting and being infected.
- To this end, the national and local governments will remind the public of the need for routine infection control measures, and take measures to support the public's efforts to prevent infection. In addition, efforts must be made to reduce the number of infected people so as not to increase the numbers of severe cases and deaths, as much as possible. Furthermore, further efforts should be made to reinforce the medical care provision system, and reduce the burdens on medical institutions and public health centers.
- 1. Further promotion of vaccinations
- In a case-control study investigating the efficacy of the SAR-CoV-2 vaccine in Japan, the prophylactic effect against the disease at 5 months after the second vaccination was low compared to unvaccinated cases in the epidemic period of BA.5. On the other hand, 3 doses of vaccination (booster) were shown to possibly increase the prophylactic effect against the disease to a moderate to high degree. It was preliminarily reported that the relative efficacy rate of 3 doses of vaccination compared with 2 doses can be expected to a certain extent.
- Regarding the booster vaccination with "vaccine for the Omicron variant," it will be prepared for use after the middle of October this year, targeting those who have completed the initial vaccination.
- For the fourth vaccination, it is necessary to continue efforts to provide earlier vaccination for eligible persons (elderly people aged 60 years and older, and those aged less than 60 years at risk for severe illness, etc.) for prophylaxis against exacerbation. Considering the ongoing spread of infection, workers at medical institutions, facilities for elderly people, etc. where many individuals who are at high risk of becoming severely ill gather, have also been included in those who are eligible for vaccination.
- Vaccination with recombinant protein may be selected for up to the third vaccination. It has been confirmed that a third vaccination restores the attenuation over time, of both the preventive effect against the Omicron variant and that against aggravation conferred by the first vaccination. Considering the current infection status, it is necessary to promote consideration of the first and third vaccinations at the earliest possible time.
- Regarding vaccination of children (5-11 years old), the Immunization and Vaccine Section Meeting considered that it was appropriate to impose an obligation to make efforts to vaccinate children, as a certain level of knowledge has been acquired during the spread of the Omicron variant.
- 2. Use of tests
-
Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, the national and local governments are required to secure a system that enables testing, and further utilize testing.
- [The Elderly]
- Frequent tests (about 2 or 3 times a week for facility workers) are required for workers at facilities for the elderly.
- Depending on the circumstances in the area, testing at appropriate occasions is recommended for users of facilities for elderly people.
- [Children]
- Depending on the circumstances in the area, if a cluster occurs it is necessary to carry out frequent testing of teachers and staff at nursery schools and kindergartens.
- At the discretion of local governments and schools, it is necessary to thoroughly observe health, test those with some symptoms, and prevent outbreaks while allowing participation in club activities such as tournaments and school trips.
- [Young people]
- Preliminary testing is further recommended when having a meal with a large number of people or when interacting with elderly people.
- Establishment of a self-testing system for fever outpatients should be further promoted, in which patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- In order to promote these efforts, it is important for the government to provide a stable supply including distribution, by purchasing antigen qualitative test kits, distributing them to prefectural governments, and providing coordination support.
-
- 3. Effective ventilation
- Based on the recommendations of the 17th meeting of the Novel Coronavirus Subcommittee, it is necessary to publicize and recommend effective ventilation methods in the summer when ventilation becomes insufficient due to the use of air conditioners (how to create airflow considering aerosols, installation of partitions that do not block airflow, etc.).
- 4. Securing a medical care provision system
- In preparation for further spread of infection, prefectural governments must take measures to avoid overcrowding of beds and fever outpatient sections with the support of the national government.
- Immediate responses such as securing beds, and the development of temporary medical facilities that play the role of supplementing hospital beds
- Making appropriate adjustments so that patients requiring inpatient treatment can be hospitalized preferentially, performing frequent tests at facilities for elderly people, etc., and further strengthening medical support
- Securing and expanding logistical support hospitals, and improving the hospital turnover rate, such as by dissemination of the standard for early discharge of 4 days, as a rule
- Promotion of effective and less burdensome measures against infection, such as flexible and efficient use of hospital beds through zoning of each hospital room
- Establishment of a self-testing system for fever outpatients should be further promoted, in which patients with symptoms can self-test using an antigen qualitative test kit, and if the result is positive, they can promptly undergo health observation at a health follow-up center, etc.
- Strengthening of the supply system of the antigen qualitative test kits, and understanding and publicizing the cases of home care without going through a fever outpatient section
- Local residents should be informed that they should refrain from visiting an emergency outpatient unit only to receive a precautionary examination without symptoms, according to the actual situation in the region. In addition, in order to respond to concerns and questions at the time of worsening physical conditions, the consultation service by healthcare professionals via telephone should be thoroughly publicized, and this service should also be strengthened.
- A system of appropriate and early administration of therapeutic drugs should be established and strengthened, such as publication of the registration status of therapeutic drugs in medical care/testing institutions.
- Response to the increasing trend of ambulance transport difficulties. In addition to confirming the acceptance system for patients other than those with COVID-19, spreading awareness of heat stroke prevention and warning of increased emergency transportation due to heat stroke.
- Ensuring that workplaces and schools do not require test certificates at the start of medical treatment
- Further promote the reduction of burdens, such as hospitalization coordination and outsourcing/unification of operations by the hospitalization coordination division, so that public health center operations will not be strained.
- 5. Surveillance
- Deterioration of the accuracy of current surveillance is a concern due to prioritization of notification items, delays in testing and diagnosis/reporting due to the spread of infection, and changes in healthcare-seeking behavior. It is necessary to promptly promote consideration of effective and appropriate surveillance to grasp the epidemic status. It is also necessary to continue monitoring the trends of variants through genomic surveillance.
- 6. Re-inspection and implementation of basic infection control
- Re-inspection and implementation of the following basic infection control measures are needed.
- Continue proper wearing of nonwoven masks, hand hygiene, thorough ventilation, etc.
- People with symptoms such as a sore throat, cough, and fever should refrain from going out.
- Avoid situations with a high risk of infection, such as the three Cs, congestion, or loud voices.
- Refer to guidelines for hospital visits and use of an ambulance.
- Eating and drinking should be done with as few people as possible, and masks should be worn except while eating and drinking.
- To reduce the chances of contact as far as possible, it is necessary for measures at the workplace, such as again promoting the use of telework.
- Organizers of events, meetings, and such should fully evaluate the epidemic situation and risk of infection in the area, and consider whether or not to hold the meeting, and if it is held, measures should be taken to minimize the infection risk.
<< Reference: Findings on the characteristics of the Omicron variant and its sublineages >>
- [Infectivity/transmissibility]
It has been confirmed that compared to the Delta variant, the generation time has shortened to approximately 2 days (approximately 5 days for Delta). The doubling time and incubation period have also shortened, the risk of re-infection and secondary infection after infection has increased, and the speed of infection spread is very fast. According to the reported data, pre-symptomatic transmission has probably occurred to some extent as with the previous strains.
- [Place/route of infection]
In Japan, many cases of infection have occurred through the same opportunities as before (spending time indoors in locations with inadequate ventilation, eating and drinking, etc.), and infection is considered to have occurred via the same routes as before (droplets adhering to mucosa, aerosol inhalation, contact infection, etc.).
- [Severity]
It has been suggested that infection with the Omicron variant presents a lower risk of hospitalization or aggravation than the Delta variant. However, analyses to date show that the fatality due to infection with the Omicron variant is higher than that due to seasonal influenza. It is also suggested that the incidence of pneumonia is higher than that of seasonal influenza, but given the limited data, it needs to be investigated by various analyses. The death toll from the previous outbreak compared to last summer's outbreak had a higher proportion of people aged 80 and over. It is reported that there are many cases in which the new coronavirus infection is not the direct cause of death, for example, people who have been in a facility for the elderly before the infection are infected and die due to the worsening of the underlying disease. Attention should also be paid to worsening of the condition of elderly infected people and infected people with an underlying disease, and to the onset of heart failure and aspiration pneumonia.
- [Duration of viral shedding]
Viral shedding in individuals infected with the Omicron variant decreases over time. In patients with symptoms, it has been shown that the possibility of viral shedding is low from 10 days after the date of onset, and that no shedding is observed after 8 days from the date of diagnosis in those without symptoms.
- [Vaccine effect]
For infection with the Omicron variant, the preventive effects of a first vaccination against infection and disease onset are markedly reduced. Its preventive effect on hospitalization is reported to be maintained at a certain level for the first 6 months, but subsequently decreases to 50% or less. On the other hand, it has been reported overseas that a third vaccination restores the infection-preventing effect, onset-preventing effect, and hospitalization-preventing effect against infection by the Omicron variant, and information on how these vaccine effects are attenuated after a third vaccination has become available. Regarding the fourth vaccination, it has been reported that while the preventive effect against aggravation was not reduced for 6 weeks, the preventive effect against infection lasted only for a short time.
- [Omicron variant sublineages]
Worldwide, the proportion of the BA.5 lineage is increasing, suggesting that this lineage is superior to the BA.2 lineage in terms of causing an increase in the number of infected people. The number of positive tests is on the rise globally, as replacement by the BA.5 lineage proceeds. The BA.5 lineage has shown a tendency to escape existing immunity compared with the BA.1 and BA.2 lineages, but no clear findings on the infectivity have been shown. The effective reproduction number of the BA.5 lineage calculated based on the data of Tokyo was about 1.27 times that of BA.2. It was also estimated that it was about 1.3 times higher in samples collected from private testing institutions nationwide.
According to the WHO report, the findings accumulated from multiple countries indicate that there is no increase in the severity of the BA.5 lineage compared to existing Omicron variants. On the other hand, the pathogenicity of the BA.5 lineage is reportedly higher than that of the BA.1 and BA.2 lineages, based on Japanese laboratory data, but it has not been confirmed clinically at this time. Although it is unknown whether it is due to the traits of the BA.5 lineage, it should be noted that the numbers of inpatient cases and severe cases are increasing in countries where the number of infected people is increasing mainly in the BA.5 lineage. According to genomic surveillance in Japan, the detection rate of the BA.5 lineage is increasing, and the previous dominant variant was replaced with this lineage.
In addition, the BA.2.75 lineage, which has been reported mainly in India since June, has been detected in Japan. However, no clear findings have been obtained overseas regarding its infectivity or severity, compared with other lineages. It is necessary to continue to collect and analyze the situation and findings in other countries regarding these characteristics of the virus, and to continue monitoring by genome surveillance.
Figures (Number of new infections reported etc.) (PDF)